ABSTRACTS
VS ASM 2024 prize winning Abstracts
The Vascular Societies’ Annual Scientific Meeting 2024, in conjunction with the VSGBI, BACPAR, SVN and CSVS, took place at DoubleTree by Hilton, Brighton, on the 27th-29th November 2024. Here are the 2024 prize winning abstracts.
VS – Sol Cohen Founders Prize
The Natural History of Splenic Artery Aneurysms: A Decade’s Experience of Surveillance and Management at a Large Tertiary Vascular Unit
Mr. Robert Leatherby1, Mr. David Li1, Mr. James Budge1, Dr Adelola Oseni2, Dr Rose Howroyd2, Professor Peter Holt1, Mr. Iain Roy1
1St George’s Vascular Institute – St George’s University Hospital NHS Foundation Trust / St George’s University of London, London, UK, 2 Interventional Radiology Department, St George’s University Hospital NHS Foundation Trust, London, UK
Background
Splenic artery aneurysms (SAAs) are the commonest visceral artery aneurysm. Their natural history is poorly defined and guidelines for their surveillance and management provide weak recommendations based on moderate quality evidence. We present one of the largest retrospective SAA series.
Methods
All patients reported to have a SAA between 2012 and 2021 inclusive at a single centre were identified through a search of radiology records. These data were combined with clinical electronic patient records and follow-up scans to determine a natural history.
Results
162 patients with SAA were identified, 73% female with a mean age of 71 years (SD 14) at index scan. The mean maximal SAA diameter in any plane was 15.7mm (range 6-62mm), 88% were calcified, 1% pseudo-aneurysmal. The morphology for 88% was saccular, 4% fusiform and 8% indeterminate.
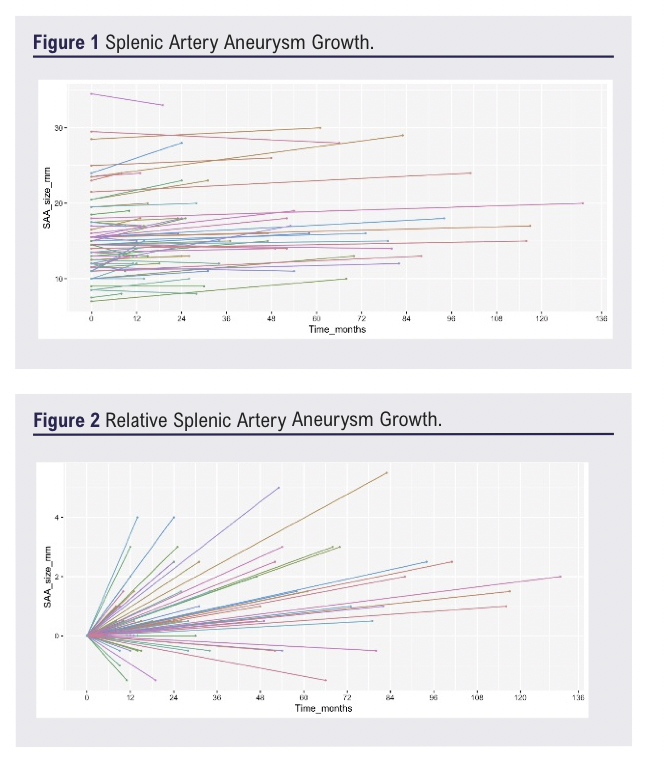
Sixty-five patients underwent further imaging, 20 within a formal SAA surveillance programme. The mean time between index and final scan was 3 years and 5 months with a mean SAA growth of 0.33 mm/year (Figure 1&2).
Five SAAs underwent intervention, 1 under surveillance, 4 de-novo: 2 for rupture. Four underwent coil embolisation (1 requiring repeat embolisation with N-butyl-cyanoacrylate) and one underwent splenectomy. There were only 2 ruptures in the cohort, neither under surveillance, both were treated successfully. There were no SAA related deaths.
Conclusion
SAAs predominate in an elderly female cohort, rarely rupture and demonstrate a slow rate of growth at 0.33mm per year. Consideration should be given to lengthening the surveillance interval in stable SAAs to 3-5 years.
VS – BJS Prize
Surgical Site Infections in Major Lower Limb Amputation: An International Multicentre Audit (SIMBA).
Miss Ismay Fabre1, The SIMBA Collaborative
1South East Vascular Network, Cardiff, United Kingdom
Introduction
Surgical Site Infection (SSI) after major lower limb amputation (MLLA) significantly affects function, mobility, morbidity and mortality alongside broader impacts on healthcare services. Limited data exists on incidence, prevention and management. Improving clinical outcomes and wound healing have been identified as research priorities for MLLA patients.
Methods
SIMBA is an international, prospective, collaborative audit. Data were collected for consecutive patients undergoing MLLA over 8 months, with 30-day follow-up. Outcomes included comparing current practice against published recommendations, incidence of SSI, wound dehiscence, revision, mortality, adjunct use, and SSI predictors.
Results
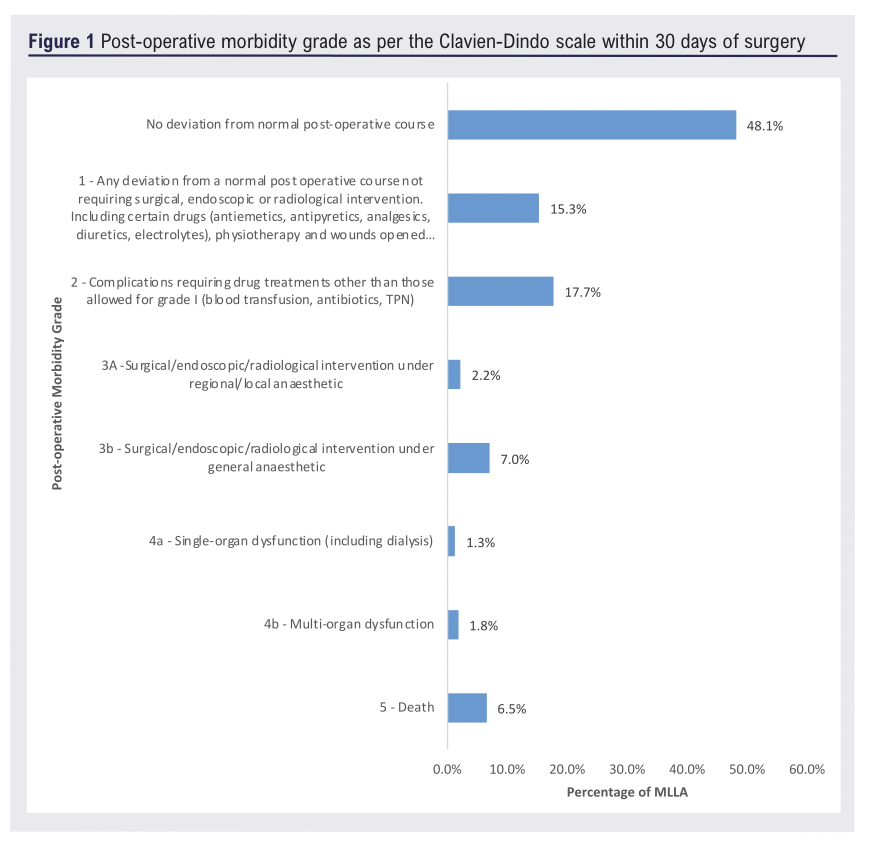
Validated data for 940 MLLA from 33 centres (UK (24), Europe (7), Australasia (1) and Asia (1)) were collected, comprising 48.0% above-knee, 3.2% through-knee and 48.6% below-knee amputations. The indications for amputation included ischaemia (52.8%), uncontrolled infection (24.1%), breakdown of previous amputation (6.4%), extensive tissue loss (13.3%) and other (3.2%). 66.2% received prophylactic post-operative antibiotics, with a mean duration of 5.8 days. The incidence of SSI and wound breakdown were 10.0% and 14.7%, respectively. Within those who developed SSI(n=94); 31.6% resulted in sepsis, and 15.8% required critical care. In total, only 48.1% of MLLA experienced no deviation from normal post-operative course, with 9.2% requiring further intervention. 30-day mortality was 6.5% (Figure 1).
Conclusion
SSI and wound breakdown after MLLA are frequent complications with significant sequelae, resulting in high rates of re-intervention, increased morbidity and mortality. SIMBA, which to our knowledge is the largest international collaborative study of its kind, highlights the need for strategies to minimise the incidence of SSI, to improve patient outcomes and reduce burden on healthcare systems.
VS – Poster Prize
The incidence of surgical site infection following major lower limb amputation: A systematic review
Miss Nina Al-Saadi1, Mr. Khalid Al-Hashimi2, Mr. Matthew Popplewell1, Miss Ismay Fabre3, Mr. Brenig Gwilym3, Miss Louise Hitchman4, Professor Ian Chetter4, Mr. David Bosanquet3, Mr. Michael Wall1
1Black Country Vascular Network, 3Colchester Hospital, 3South East Wales Vascular Network, 4Hull York Medical School
Introduction
Surgical site infections (SSIs) following major lower limb amputation (MLLA) in vascular patients are a major source of morbidity. The objective of this systematic review was to determine the incidence of SSI following MLLA in vascular patients.
Method
This review was prospectively registered with the International Prospective Register of Systematic Reviews (CRD42023460645). Databases were searched without date restriction using a pre-defined search strategy.
Results
The search identified 1427 articles. Four RCTs and 21 observational studies, reporting on 50 370 MLLAs, were included. Overall SSI incidence per MLLA incision was 7.2% (3628/50370). The incidence of SSI in patients undergoing through-knee amputation (12.9%) and below-knee amputation (7.5%) was higher than the incidence of SSI in patients undergoing above-knee amputation, (3.9%), p<0.001. The incidence of SSI in studies focusing on patients with peripheral arterial disease (PAD), diabetes or including patients with both was 8.9%, 6.8% and 7.2%, respectively.
Conclusion
SSI is a common complication following MLLA in vascular patients. There is a higher incidence of SSI associated with more distal amputation levels. The reported SSI incidence is similar between patients with underlying PAD and diabetes. Further studies are needed to understand the exact incidence of SSI in vascular patients and the factors which influence this.
VS – The Richard Wood Memorial Prize
Anxiety levels in men in Abdominal Aortic Aneurysm (AAA) surveillance: a cross-sectional survey to investigate the prevalence of psychosocial consequences of AAA in men in surveillance
Ms. Jane Hughes1, Mr. Akhtar Nasim2, Mr. Alan Elstone4, Dr Jo Hall3, Mrs Elizabeth Lumley1, Mr. Niall Macgregor-Smith1, Professor Jonathan Michaels1, Mr. Stephen Radley2, Dr Phil Shackley1, Professor Gerry Stansby5, Dr Emily Wood1, Professor Alicia O’Cathain1
1University of Sheffield, Sheffield, United Kingdom; 2Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom; 3Derbyshire Community Health Services NHS Foundation Trust, Bakewell, United Kingdom, 4University Hospitals Plymouth NHS Trust, Plymouth, United Kingdom, 5The Newcastle Upon Tyne University Hospitals NHS Foundation Trust, Newcastle Upon Tyne, United Kingdom
Introduction
Abdominal Aortic Aneurysm (AAA) is a potentially fatal condition. There are approximately 3500 deaths annually in England and Wales following AAA rupture. The NHS AAA Screening Programme undertakes surveillance on men with small AAA’s. There are potential harms as well as benefits associated with screening. This study investigates the prevalence of the psychosocial consequences of AAA in men in surveillance, and how these consequences vary by characteristics of men, their AAA and their screening frequency, using generic and AAA-specific measures of quality of life.
Methods
We conducted a cross-sectional postal survey of 1161 men in surveillance with five providers in England. The survey comprised the ePAQ-AAA, the Psychological Consequences of Screening Questionnaire (PCSQ), the EQ-5D-5L, socio-demographic questions and a free text section.
Results
The response rate was 64% (734/1161). Anxiety levels related to AAA varied by size, rate of growth, screening frequency and men’s characteristics. For example, mean scores for the ePAQ-AAA scale measuring anxiety ranged from 15.1 for a small AAA (3.0 – 4.0cm) to 28.1 for a AAA over 5.0cm in diameter (p<0.001). Men with fast growing AAA’s had higher mean scores than those with slow or non-growing AAA’s (40.7 vs 13.1) (p<0.001). Men from the most socially deprived areas had higher anxiety scores than those in the least deprived areas (25.1 v 17.3) (p<0.001).
Conclusion
Any intervention aimed at managing anxiety can be targeted at men in three monthly surveillance or with fast growing AAA’s and must be acceptable to men from socially deprived areas.
VS – Venous Prize
Characterising variations in venous thromboembolism prophylaxis practice in orthopaedic surgery: a cross-sectional survey
Mr. Shahaab Shameem, Dr Francesca Siracusa, Mr. Joseph Shalhoub, Professor Alun Davies
Imperial College London, United Kingdom,
Orthopaedic surgery can predispose patients to venous thromboembolism, however literature highlights the limited prescribing of guideline-appropriate thromboprophylaxis.1–7 Differing physician opinions and controversies in evidence creates variation in guidance, potentially challenging unified prescribing. This study aims to characterise variability in thromboprophylaxis prescribing within orthopaedics.
A scenario-based survey was designed on Qualtrics.com, comprising five total knee arthroplasty (TKA) scenarios and five knee arthroscopy scenarios. The survey was distributed to surgeons and haematologists via professional associations to elicit routine thromboprophylaxis practices. Responses were collated over six weeks. Descriptive statistics and Fisher’s exact tests evaluated the impact of risk factors on thromboprophylaxis strategy.
30 responses were analysed. Most respondents prescribed mechanical prophylaxis for TKA (83.3%, n=25) and knee arthroscopy (70.4%, n=19), with variability in the type and duration selected. Pharmacoprophylaxis use varied in knee arthroscopy, with further debate regarding the duration selected. In TKA, respondents were more likely to modify thromboprophylaxis for a history of deep vein thrombosis (DVT) or low platelet count than for other risk factors (p<0.05). In knee arthroscopy, thromboprophylaxis changes were more likely for a history of DVT (p<0.01).

Variation in the type and duration of thromboprophylaxis was documented, which may be associated with the conflicting evidence supporting certain prophylactic agents.8–15
VS – Medical Student Prize
Using Thromboelastography to compare post-operative anticoagulation: Rivaroxaban and Apixaban demonstrate similar clot strengths in Peripheral Arterial Disease patients
Miss Aaliya Ashik1,2, Miss Lois Owolabi2,3, Dr Adriana Rodriguez2, Mr. Shiv Patel2, Dr Isabella Cieri2, Dr Leela Morena2, Mr. Mohit Manchella2,3, Miss Enya Wang2,4, Dr Anahita Dua2
1University Of Manchester, Manchester, United Kingdom; 2Massachusetts General Hospital, Boston, United States of America; 3Harvard Medical School, Boston, United States of America; 4University of Rochester School of Medicine and Dentistry, Rochester, United States of America
Introduction
The VOYAGER trial demonstrated that adding low-dose Rivaroxaban improves peripheral arterial disease (PAD) post-revascularisation outcomes but did not study the effect of other anticoagulants. This study utilised Thromboelastography with Platelet Mapping (TEG-PM) to objectively compare the impact of Rivaroxaban and Apixaban on clot strength (MA-ADP) to determine if there was a difference between medication regimens.
Methods
Patients with PAD undergoing a revascularisation procedure between 2021-2023 were prospectively evaluated. TEG-PM samples taken one-month post-operatively were compared based on patient anticoagulation (Apixaban and Rivaroxaban) and antiplatelet regimen. Descriptive statistics characterised the anticoagulant groups, with Chi-square or Fisher’s exact tests comparing discrete data such as demographics and co-morbidities. Mann-Whitney U testing compared MA-ADP values between groups where Gaussian distribution was not seen, and Welch’s t-test was used where Gaussian distribution was seen.
Results
Sixty-eight samples were analysed. 32% were on Rivaroxaban, and 68% were on Apixaban. No significant difference in the MA-ADP was noted between Rivaroxaban and Apixaban groups when antiplatelet use was not controlled for (46.9mm (IQR 34.5) vs 45.1mm (IQR 34.2), p= 0.7). Similarly, no significant difference was noted between Rivaroxaban and Apixaban when patients were taking dual antiplatelet therapy (37.8mm ±16.7 vs 42.8mm ±19, p=0.5), Aspirin monotherapy (46.4mm ±20.8 vs 44.3mm ±14.2) or Clopidogrel monotherapy (58.3mm (IQR 43.2) vs 45.9mm (IQR 42.8), p>0.9).
Conclusion
No significant difference was noted in clot strengths between PAD patients taking Apixaban vs Rivaroxaban. This is clinically useful when considering post-operative thromboprophylaxis prescribing, as both medications are equally efficacious.

SVN – James Purdie Prize
Empowering Patients: A Project for Raising Awareness of Peripheral Arterial Disease (PAD) and the Development of the Claudication Pathway
Miss Lauren Lynch, Mrs Zoe Noakes, Mrs Ellena Smedley, Mr. Edward Lopez, Mrs Angela Iles
University Hospital Coventry and Warwickshire, Coventry, United Kingdom
This project aims to address the under diagnoses and under treatment of PAD and its associated symptom, intermittent claudication, by engaging patients, healthcare professionals, and the broader community in awareness-raising activities. Through education, patient empowerment, and advocacy, we aspire to improve early detection, management, and outcomes for individuals living with PAD.
The vision the Vascular Nursing Team had was:
• To raise awareness about PAD and its associated symptom, claudication, among both the general population and healthcare professionals.
• Establish a clear pathway for the diagnosis, management, and treatment of PAD and claudication.
• Empower patients with PAD to actively participate in their healthcare journey and advocate for improved access to resources and support.
We established areas of waste within the current service and conducted audits of the current clinic set up to identify areas of improvement. Patient forums were introduced for them to share their views and ideals. Surveys were taken and feedback was welcomed. Patient focus groups shall continue as the team recognises that patients provide valuable insights into the usability, appropriateness, and impact of the service on their experiences and outcomes.
The long-term benefits in terms of improved patient outcomes by preventing disease progression, reducing hospitalisations, and minimising the need for invasive procedures results in reduced healthcare costs. By reducing waste within the previous service, along with reducing wait times for initial appointments for patients, the clinical capacity has increased by more than 150% resulting in a financial gain of over £50,000 per year for the Trust.


SVN – Poster Prize
Multicomponent interventions to support adherence to guideline-recommended therapy in patients with peripheral arterial disease
Mrs Smaragda Lampridou1,2, Miss Tania Domun1, Miss Javiera Rosenberg1, Professor Alun Huw Davies1,2, Professor Mary Wells1,2, Dr Gaby Judah1
1Imperial College London, 2Imperial College Healthcare NHS Trust
Introduction
Adherence to guideline-recommended therapies in peripheral arterial disease (PAD) patients remains low. Single-component interventions addressing either smoking, exercise or medication adherence have demonstrated some efficacy. However, given the complexity of the PAD treatment plan, multi-component interventions are essential for comprehensive patient management. This scoping review systematically synthesized information on multi-component interventions for PAD patients.
Methods
A systematic search was conducted in Embase, MEDLINE, Cochrane Library, APA PsycINFO, CINAHL, Web of Science Core Collection, ProQuest and Google Academic, to identify primary research describing multicomponent interventions to support treatment adherence in PAD patients, published between 2007-2024. A narrative synthesis was reported using the Template for Intervention Description and Replication (TIDieR) checklist and the Behavioural Change Techniques (BCT) Taxonomy.
Results
This review included 15 studies including 2,462 PAD patients (60.4% male). Only two interventions targeted all PAD therapies. Key intervention components included structured exercise (12/15) and education programmes (10/15). Most interventions were delivered by multidisciplinary teams in hospital settings over three months. Only one study reported employing behavioural theories in its development, and most interventions (14/15) focused on the BCT “instruction on how to perform a behaviour” rather than diverse BCTs. No interventions significantly increased adherence to all PAD therapies.
Conclusion
Few interventions target all behaviours; with no evidence of holistic support. Not enough studies measured the intervention’s impact on adherence, hindering recommendations on effective intervention characteristics. Most interventions lacked behavioural science approaches and were not designed to address specific adherence determinants. Future interventions should incorporate behavioural strategies to maximise patient benefit.
CSVS – Best Scientific Abstract
Ultrasound based turbulence quantification can predict intimal hyperplasia development in arteriovenous fistula.
Mr. Matthew Bartlett1
1Royal Free London NHS FT, London, UK, 2UCL, London, UK
Introduction
Imaging surveillance does not offer significant improvements to long term arteriovenous fistula (AVF) patency, but the haemodynamic information obtained using Doppler ultrasound, may hold the key to developing improved monitoring techniques.
Objectives
• Develop a simple tool for analysing the complex haemodynamic data contained within a Doppler spectrogram and quantify the level of turbulence present.
• Validate the tool using patient specific in-silico simulations, and in-vivo trials.
Materials & Methods
Patients with newly created AVF underwent duplex scanning post-surgery. Cardiac gated audio recordings of the Doppler shifted frequency spectrum were obtained and an ensemble averaging technique was employed to extract the frequencies relating to turbulent components of the flow field. Ultrasound Turbulence Intensity Ratio (USTIR) was calculated in different regions of the flow circuit and compared with distribution of oscillatory shear index (OSI) on the computational simulations, and with neointimal hyperplasia (NIH) development on the 10-week maturation scan.
Results & Summary
Distribution of ultrasound-based turbulence intensity ratio corresponds with regions of elevated oscillatory shear stress and accelerated NIH formation. ROC curve analysis found a USTIR >6.4 of the pre-maturation scans, could predict development of haemodynamically significant NIH at 10 weeks with a sensitivity of 87.5% and a specificity of 80%.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;5(1):38-45
Publication date:
November 26, 2025











