ORIGINAL RESEARCH
Outcome measurement for vascular amputee patients: a scoping survey of UK clinical practice
Essop-Adam A,1–3 Singh SJ,3-5 Haunton VJ,1 Meffen A,1,6 Sayers RD1–3
Plain English Summary
Why we undertook the work: Using appropriate physical assessment tests with patients who have undergone an amputation due to vascular disease is important to patients and healthcare professionals. They are used to assist with setting patient goals and monitoring how a patient is progressing when they are undergoing treatment or rehabilitation. At the moment it is not known which physical assessment test is most useful to use with patients who do not walk or use a prosthetic limb.
What we did: Before starting the research we obtained ethical approval from the University of Leicester. We carried out a survey with healthcare professionals who currently work in the UK and used an online platform to run the survey. We asked healthcare professionals what kind of physical assessment tests they are using at the moment with patients, and how useful they find them.
What we found: Over half of the healthcare professionals who responded to the survey had over 10 years of experience working with amputees. Healthcare professionals stated that they more commonly used physical assessment tests to assess walking (89%) and less than half used assessment tests with patients who do not walk (45%). Healthcare professionals stated the assessment tests for patients do not walk are not useful when treating patients.
What this means: At the moment the available physical assessment tests are not being used frequently with the majority of patients who do not use a prosthetic limb for walking after an amputation due to vascular disease. Therefore, this study may support the development of a new physical assessment test that would be useful for patients and healthcare professionals to assist with setting patient goals and providing treatment or rehabilitation to these patients.
Abstract
Objective: Currently it is unknown whether Physical Performance Based Outcome Measures (PerBOMs) are used in clinical practice with patients who have undergone an amputation due to peripheral arterial disease. This study aims to explore the clinical use and usefulness for healthcare professionals (HCPs) and to look at the types of rehabilitation interventions being provided to amputees.
Methods: An anonymised scoping survey published online at https://www.onlinesurveys.ac.uk was used. The survey consisted of 17 questions, and all data collected were non-identifiable. Ethical approval was obtained from the University of Leicester ethics committee. Statistical analysis was completed with descriptive statistics.
Results: A total of 125 HCPs responded, of which more than half had ≥10 years’ experience working with vascular amputees (51.2%). Timed Up and Go was the most used ambulatory PerBOM by HCPs (89%) and the Basic Ambulatory Mobility Scale (45%) was the most commonly used non-ambulatory PerBOM. PerBOMs were least used before amputation (15%) and were used most frequently 6 months after amputation (59%). HCPs rated PerBOMs for ambulatory patients as being of greater usefulness than non-ambulatory PerBOMs. The most common rehabilitation interventions for non-ambulatory amputees include transfer practice (85.5%) and wheelchair training (69.6%); few provided group exercise therapy (23.2%).
Conclusions: Ambulatory PerBOMs are well known and used more frequently than non-ambulatory PerBOMs. PerBOMs for vascular amputees are not used within clinical practice due to the limited number and inadequate options of PerBOMs for non-ambulatory vascular amputees. Further research is needed in understanding the limited clinical use of existing PerBOMs. Pending further research, a new PerBOM for non-ambulatory patients may be supported to assess the physical function of amputees throughout the patient journey of vascular amputees and for goal setting in the short and longer term.
Introduction
Peripheral arterial disease (PAD) and/or diabetes is the largest cause of major amputation.1 Individuals who have undergone an amputation due to vascular disease (‘vascular amputees’) often have multiple comorbidities, are older, frail,2 have decreased physical function and live with disability following their amputation.3,4 Vascular amputees often do not wear a prosthesis for ambulation for several reasons. Factors affecting successful prosthetic wear include patients experiencing reduced physical function pre-amputation,5 multiple co-morbidities,6 altered cognitive function7 and potential problems with their contralateral limb8,9 if a unilateral amputee. This often leads to an inability to wear a prosthetic limb or unsuccessful prosthetic rehabilitation.7,10 In this paper patients who do not use a prosthetic limb for walking following an amputation due to vascular disease will be referred to as ‘non-ambulatory vascular amputees’.
Vascular amputees live with disability and require appropriate assessment of their physical function for holistic clinical management and rehabilitation with Physical Performance Based Outcome Measures (PerBOMs) throughout their patient journey and as their PAD develops.11 Using appropriate PerBOMs within clinical practice can support healthcare practitioners (HCPs) to set patient goals and monitor progression whilst receiving treatment and rehabilitation.
At present there is little guidance on which PerBOMs are best to use with the vascular amputee population. A comprehensive list of all PerBOMs that have been validated and clinimetric properties assessed with the vascular amputee population has been produced in a systematic review of all previous literature.12 This paper identifies that only four PerBOMs are suitable for the non-ambulatory amputee population: Amputee no Prosthesis (AMPnoPro),13 Transfemoral Fitting Predictor (TFP),14 One Leg Balance Test (OLBT)15 and Basic Amputee Mobility Score (BAMS).16 However, it is unknown which of these validated outcome measures are being used within clinical practice in the UK and which PerBOMs clinicians find useful. It would be important to determine whether there is a mismatch between published research and current clinical practice.17
Primarily, this survey aims to explore the current use of outcome measures in clinical practice with vascular amputees in order to inform clinicians which PerBOMs are most useful clinically and for future research projects developing PerBOMs for non-ambulatory vascular amputees.
Secondly, this survey aims to explore variation in existing rehabilitation services for non-ambulatory vascular amputees and the type of rehabilitation interventions being delivered to this patient population.
Methods
This paper was written in accordance with the CHERRIES checklist.18 An anonymous scoping survey was produced with the aid of a list of all PerBOMs from a systematic review.12 Ethical approval was sought and granted from the University of Leicester ethics committee (reference: 27972-aea19-ls:cardiovascularsciences).
The survey topics and questions were designed and refined with key stakeholders who identified themes and questions relevant to this patient population. Key stakeholders consisted of HCPs working with vascular amputees and researchers. The initial version was piloted to a convenience sample of HCPs and researchers. Changes were suggested and made to the survey questions and format prior to publishing the survey online. Due to the exploratory nature of this scoping survey, the survey was not validated prior to circulation.
All participants completed the survey online at https://www.onlinesurveys.ac.uk, where the responses were automatically captured by the website. All data collected were non-identifiable; each responder was provided with a unique study ID number. The data were stored in the University of Leicester secure research file store on University of Leicester password-protected computers in locked offices.
Seventeen questions were produced for the survey. The list of online questions is shown in Appendix 1 online at www.jvsgbi.com. Adaptive questioning including conditionally displayed questions based on the responses was used (Appendix 2 online at www.jvsgbi.com) to reduce the number of questions and complexity of the survey. To reduce missing data or incomplete survey responses, all questions that appeared to the participant were mandatory. Some questions provided a ‘not applicable’ answer to limit non-response. Participants were able to use the back button to change their answers.
The sample was distributed to a convenience sample of HCPs through email networks including local and national networks. Further convenience sampling methodology was used by distributing the survey through national email networks including the British Association of Charted Physiotherapists in limb Absence Rehabilitation (BACPAR) and the British Association of Orthotists and Prosthetists (BAPO) membership lists. The survey was also advertised on X (formerly Twitter). Details of the study including the purpose of the study, approximate length of time to complete the survey and data storage information were included as a Participant Information Sheet (PIS) attached to the survey (Appendix 3 online at www.jvsgbi.com). Participation was completely voluntary, as described on the website and PIS. Informed consent on the first page of the survey was provided by participants before completing the scoping survey. Data were collected between 1 January 2021 and 30 April 2021.
Data analysis
Descriptive statistics and figures exploring participant characteristics and PerBOM use were produced using Microsoft Excel. Subgroup analysis for vascular physiotherapists only was completed with descriptive statistics as this group was the largest cohort of HCP participants. Due to the exploratory nature of the survey, statistical analysis was limited to descriptive statistics.
Results
Participant characteristics
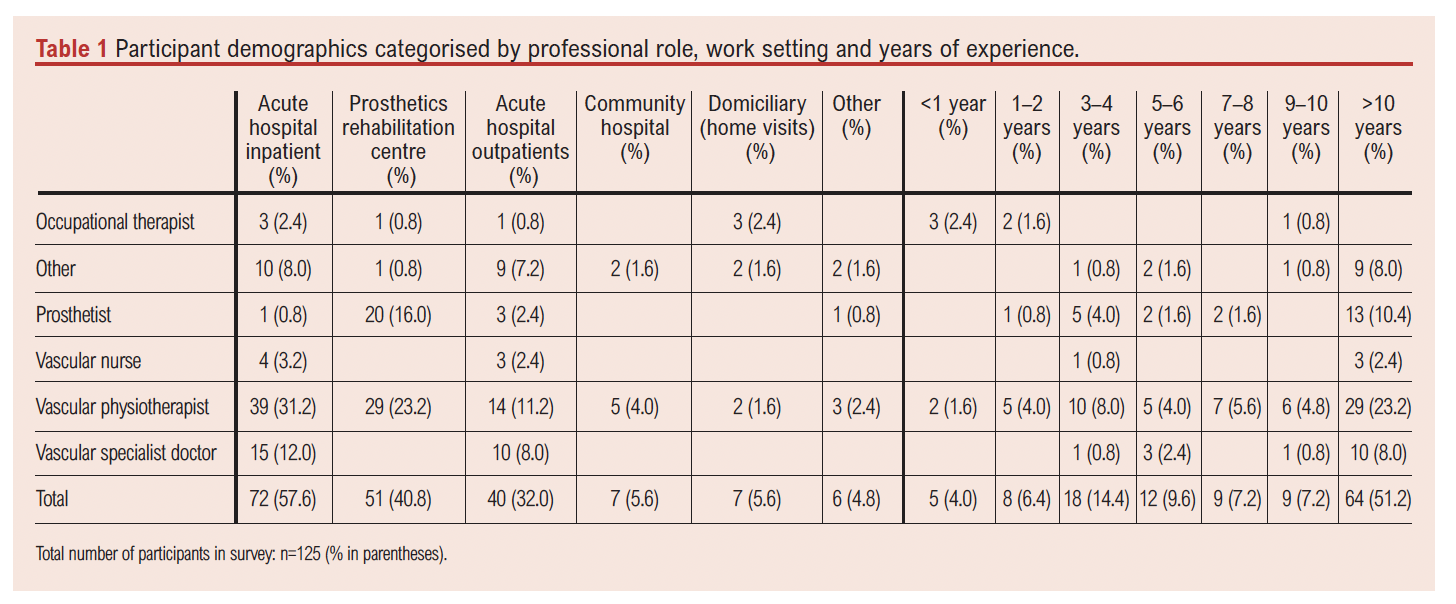
The survey was completed by 125 participants. The website initial participant information page had a view rate count of 860. Fifty-five individuals started the survey and abandoned it. Incomplete responses were not recorded. The survey was completed by a range of HCPs including vascular physiotherapists, prosthetists, vascular specialist doctors, occupational therapists, vascular nurses and other HCPs (Table 1). Vascular physiotherapists accounted for more than half of the participants and were the largest group of HCPs, and vascular nurses made up the smallest group of participants (n=4). Sixty-four (51.2%) of the participants had more than 10 years’ experience working with vascular amputees and only five (4.0%) had less than 1 year experience.
Information on the participants’ location of work was also obtained (Table 1). The largest number of participants (n=72, 57.6%) worked in an acute hospital inpatient setting and the smallest number of participants (n=7, 5.6%) worked in a community hospital or domiciliary setting. Vascular physiotherapists worked in the largest range of different settings while vascular specialist doctors and vascular specialist nurses both primarily worked in inpatient or outpatient acute hospital settings. The majority of prosthetist responders worked in prosthetic rehabilitation centres, with limited numbers in other clinical areas.
Use of outcome measures
The participants were familiar with different types of PerBOMs including Patient Reported Outcome Measures (PROMs), PerBOMs and Clinically Reported Outcome Measures (CROMs) (Figure 1). Overall, the highest number of participants selected familiarity with PROMs (n=102), with slightly fewer participants selecting CROMs (n=98) and PerBOMs (n=94). For all professional groups except prosthetists and physiotherapists, PROMs were the most familiar type of outcome measure.
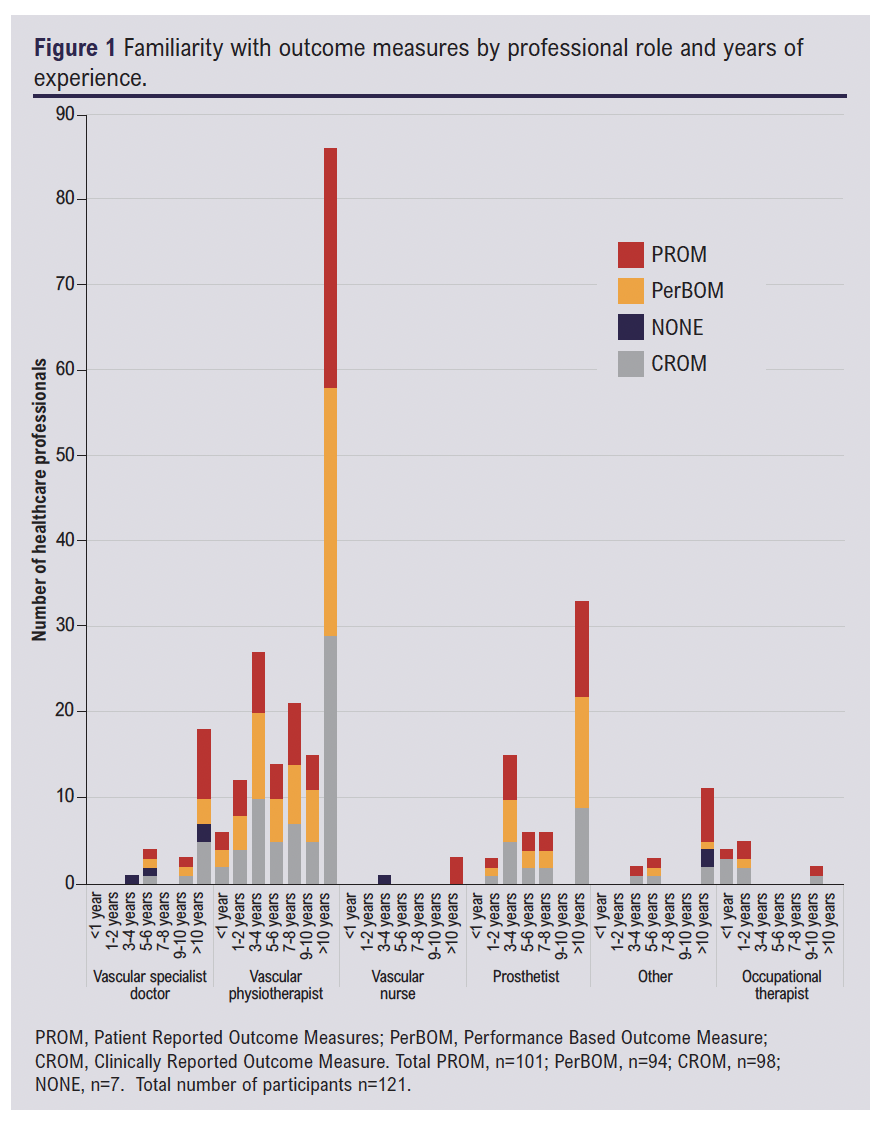
We also explored how often participants used PerBOMs in clinical practice in this survey (Figure 2): 39 (33%) stated that they ‘never use’ PerBOMs in their clinical practice, 25 (21%) and 24 (20%) stated using PerBOMs ‘sometimes’ or ‘most of the time’, and 33 (27%) stated that they ‘always’ used PerBOMs.
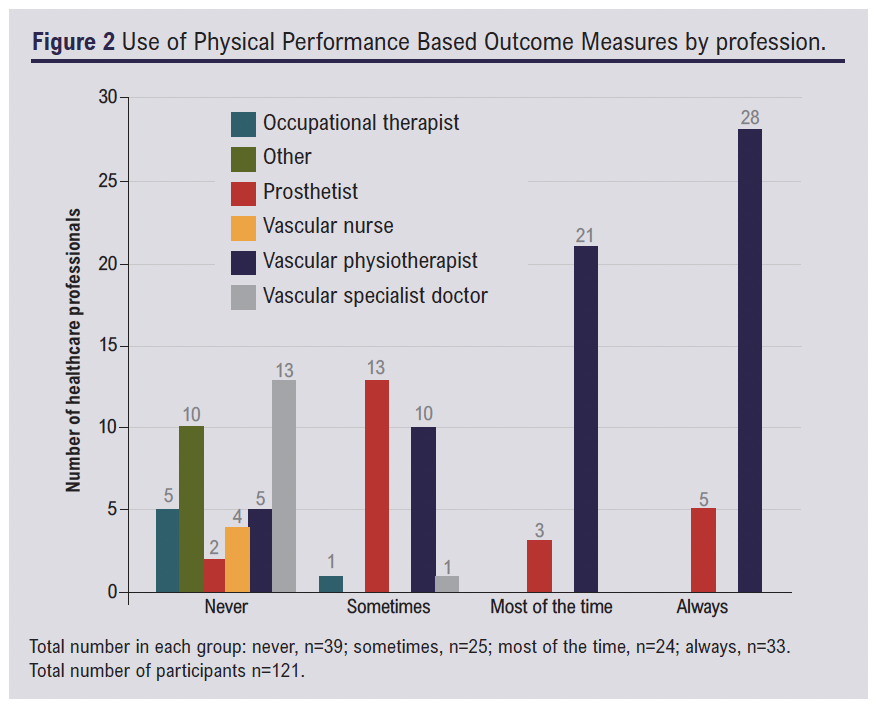
Eighty-two participants, the majority of which were vascular physiotherapists and prosthetists, identified using PerBOMs ‘sometimes’, ‘most of the time’ or ‘always’. These 82 participants proceeded to continue with questions regarding PerBOM rating and evaluation due to the conditional questioning method of displaying questions in the survey.
Of the previously identified PerBOMs, participants were requested to identify which of them are being used clinically in practice (Figure 3). Timed Up and Go (TUGT) was the most used PerBOM identified (89%). Other commonly used ambulatory PerBOMs include the 2 Minute Walk Test (2MWT), 6 Minute Walk Test (6MWT) and the Berg Balance Scale (BBS). The most commonly used non-ambulatory PerBOM was the Basic Amputee Mobility Score (BAMS) with 37 (45%) participants using this PerBOM clinically and 32 (39%) being aware of this PerBOM but not using it clinically. Other non-ambulatory PerBOMs include the Transfemoral Fitting Predictor (TFP) used clinically by 32 (39%) participants and the One Leg Balance Test (OLBT) used clinically by 28 (34%). Only 26% of participants were aware of the TFP and over a third (35%) had never heard of this PerBOM. The Amputee Mobility Predictor no Prosthesis (AMPnoPro) is the least commonly used clinically non-ambulatory PerBOM; 31 (51%) participants were aware of it but did not use it clinically. The least commonly used PerBOMs include the arm-leg ergometer, Modus trex monitor, one leg cycle test, PUMP tool and Sensory Organisation Test (SOT), all of which (except the PUMP tool) are digitally-enabled PerBOMs.

Participants ranked the PerBOMs on their usefulness out of 10, where 1 is least useful and 10 is very useful. Seventy-two participants in total scored the TUGT. The box and whisker diagram in Figure 4 shows a skew towards a higher score of between 7 and 10 for the TUGT, 2MWT and 6MWT. Minimum values varied, with a score of 2 for TUGT, 5 for the 2MWT and 3 for 6MWT. The BBS, with a median value of 7, was rated by 39 HCP participants. All four ambulatory PerBOMs had an interquartile range of around 3.
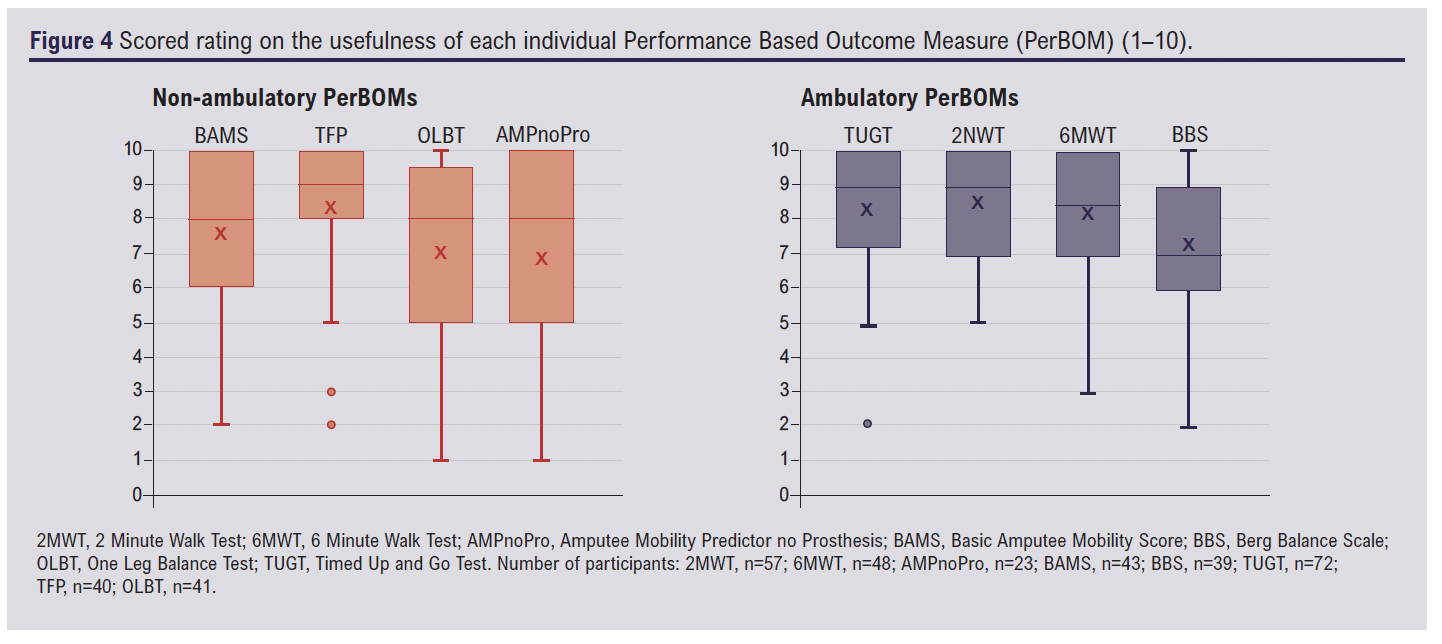
The BAMS (n=43), TFP (n=40) and OLBT (n=41) non-ambulatory measures have a similar spread of data with maximum values of 10 and minimum values of 1 and 2. Interquartile range (IQR) varied, with BAMS IQR of 4, TFP IQR of 2 and OLBT IQR of around 4. The TFP was scored by 40 participants and had an overall higher median score than all other non-ambulatory PerBOMs. The AMPnoPro (n=23) had a wide spread of data, with the largest IQR of 5.
PerBOM use (Figure 5) at different timepoints was identified. PerBOMs were used less frequently before amputation and in the early stages after amputation at 0–7 days and were used most frequently at >6 months and 1–3 months after amputation.
Vascular physiotherapists
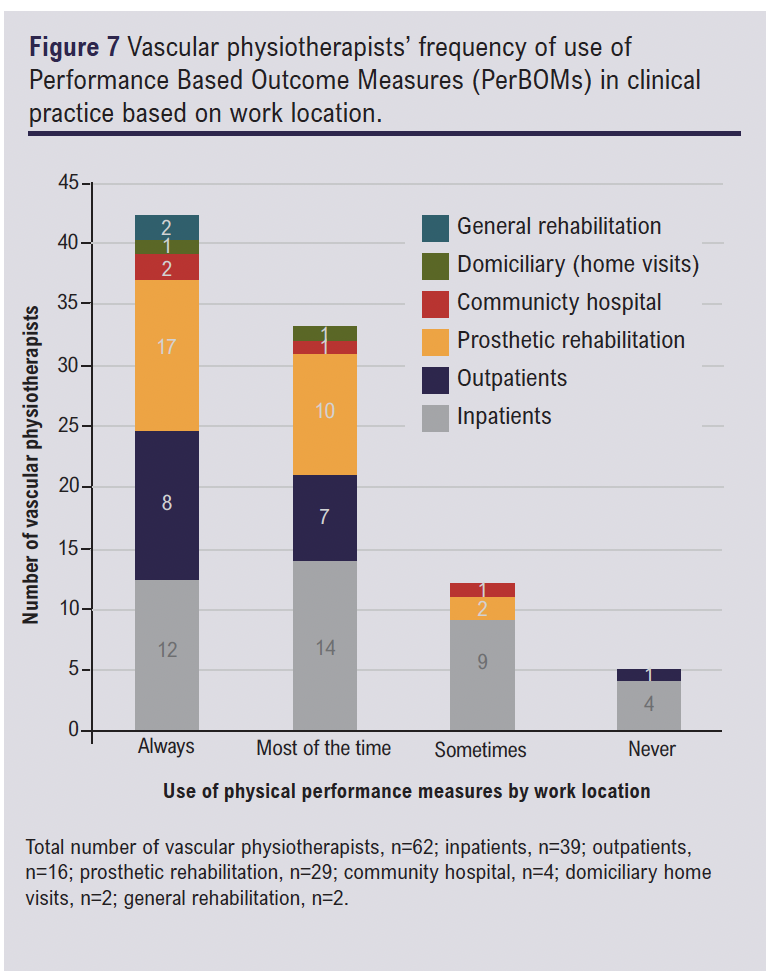
Vascular physiotherapists were the largest group of HCPs in this study, so a sub-analysis was made for this group of participants (n=64). The frequency of use of PerBOMs by vascular physiotherapists has been categorised by years of clinical experience (Figure 6) and work location (Figure 7).
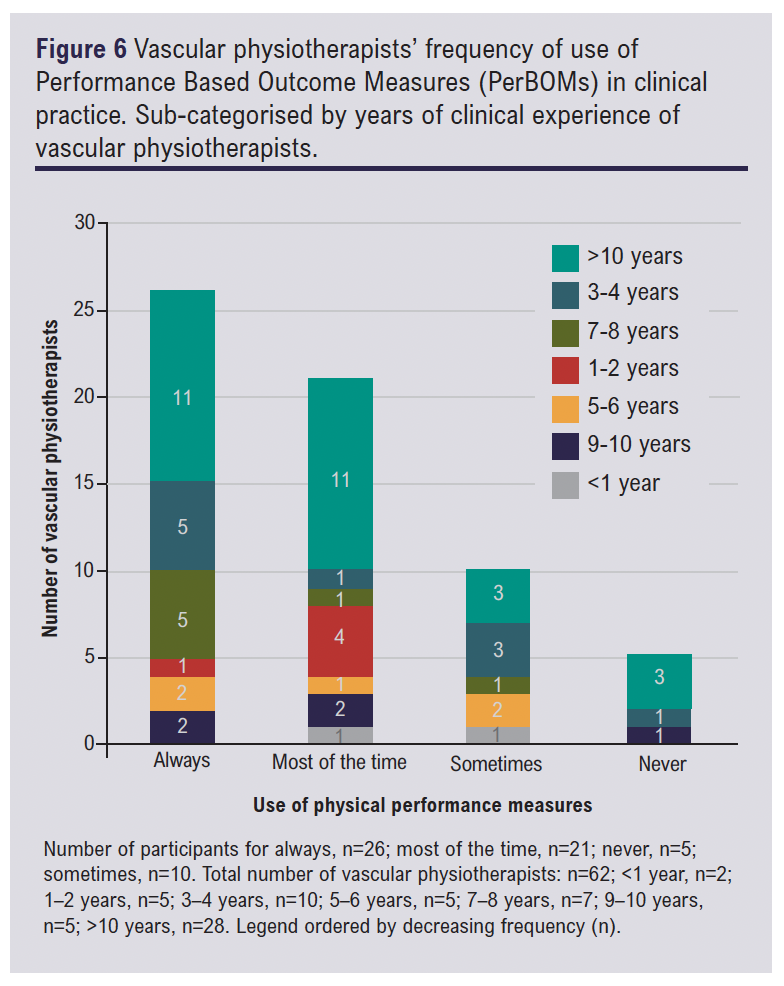
Around half of the participants had >10 years of experience (n=28). The largest number of participants (n=26) selected that they ‘always’ used PerBOMs in clinical practice, equal numbers of highly experienced vascular physiotherapists with either >10 years or 9–10 years of experience stated that they either use PerBOMs ‘always’ or ‘most of the time’, while the smallest number of participants (n=5) stated that they ‘never’ used PerBOMs.
Vascular physiotherapists have varying clinical roles in clinical practice and therefore they were able to answer that they work in more than one work location (Figure 7). The majority of vascular physiotherapists worked in the inpatient hospital setting (n=39) and the smallest number of participants worked in a general rehabilitation or home visit domiciliary setting (n=2). Participants who worked in a prosthetic rehabilitation setting were more likely to use PerBOMs; PerBOMs were used ‘always’ (n=17) and ‘most of the time’ (n=10) in clinical practice, with only minimal numbers using them ‘sometimes’ (n=2) and no participants ‘never’ using them.
However, participants who worked in an acute hospital inpatient setting demonstrated varying use of PerBOMs, with no trends towards increased or decreased frequency of use of PerBOMs in clinical practice. Additionally, around 10% of participants who worked in an acute hospital inpatient setting never used PerBOMs in clinical practice (n=4).
Rehabilitation
Rehabilitation for patients who have undergone an amputation due to vascular disease who are ambulatory and non-ambulatory is described in Appendix 4 online at www.jvsgbi.com. Few HCPs provide pre-habilitation to non-ambulatory patients (n=23) and ambulatory patients (m=26), whilst general rehabilitation is most frequently provided in total for ambulatory and non-ambulatory patients. Similar numbers of participants provided prosthetic rehabilitation, specialist amputee rehabilitation and general rehabilitation (n=54–55) to ambulatory patients.
Rehabilitation for non-ambulatory patients who have undergone an amputation at different timepoints was also explored in the survey (Figure 8). The survey identifies that rehabilitation for non-ambulatory patients is most frequently provided by HCPs at 0–7 days (n=42) and 8–28 days (n=43) after amputation. Pre-habilitation was provided by HCPs less frequently (n=29). However, the fewest HCPs provide rehabilitation to non-ambulatory patients in the longer term after amputation at 3–6 months (n=18) and >6 months after amputation (n=14).

Discussion
A range of different of HCPs have completed the scoping survey, with vascular physiotherapists making up the majority of the participant cohort. This is possible to be representative of the HCPs who are using PerBOMs in clinical practice, as physiotherapists have been using PerBOMs in clinical practice to prove clinical effectiveness since the 1990s.19,20 A large variety of HCPs completed the scoping survey, including many vascular specialist doctors and prosthetists. This represents a large range of HCPs who are involved in the clinical management and care of patients.
Previous evidence states that there are often issues with the use of PerBOMs in clinical practice when there is a lack of physiotherapist knowledge and experience of using outcome measures.21 Data in this survey suggest that PerBOMs are likely to be used by physiotherapists at all stages of clinical experience. This demonstrates that there was no relationship between the use of PerBOMs in clinical practice for vascular physiotherapists and the number of years in clinical practice, therefore indicating that clinical uptake of available PerBOMs may be due to other factors.
Work location did appear to have an influence on whether PerBOMs were used (Figure 7) as vascular physiotherapists who worked within an acute inpatient setting reported using outcome measures at varying rates. In comparison, those who worked in prosthetic rehabilitation more frequently used PerBOMs ‘always’ and ‘most of the time’. This could be expected from the busy acute hospital setting where there is little prosthetic or walking rehabilitation. Furthermore, staff are often limited on time in the acute hospital inpatient setting,22 with particular focus on patient discharge destination. This finding differs from previous work which suggested that physiotherapists were likely to use PerBOMs in all clinical settings.20
Additionally, few participants worked in a community hospital or completed domiciliary visits. Due to lack of responders in these clinical areas, we are unable to obtain representative data on them.
Previous evidence evaluating PerBOMs for this patient population is limited. A previously published systematic review recommends the AMPnoPro, TFP, OLBT and BAMS for use in clinical practice for non-ambulatory amputees.12 Based on the tasks involved, the BAMS16 would be most suited clinically for patients early after amputation in the acute inpatient hospital setting. However, despite the fact that BAMS is reportedly the most used non-ambulatory PerBOM, it is only used clinically by less than half of HCPs with non-ambulatory patients. Furthermore, although a third of participants were aware of this PerBOM, it was not chosen to be used clinically.
The notion that PerBOMs for non-ambulatory patients are unlikely to be used in clinical practice is also emphasised, with participants using PerBOMs least frequently at timepoints before amputation and 0–7 days after amputation, when patients would be non-ambulatory before and immediately after surgery.
For non-ambulatory PerBOMs the one with the highest median usefulness score is the TFP. However, the number of participants rating the TFP was around a third less than the number of participants rating the TUGT, the most commonly scored ambulatory PerBOM. Although the TFP was found to be relatively useful, this should be interpreted with caution as fewer participants rated the non-ambulatory PerBOMs compared with the ambulatory PerBOMs. There is a clear disparity between the current validated outcome measures12 and current clinical practice. This study suggests this variation could be explained by HCPs reporting limited usefulness of these outcome measures. Future research may focus on an investigation into the reasons for limited PerBOM use with non-ambulatory amputee patients. Development of a suitable, meaningful and clinically relevant new PerBOM is suggested, which may support the management of non-ambulatory patients.
The findings of this study suggest that participants were more likely to use PerBOMs if they worked in a prosthetic rehabilitation centre with ambulatory patients who are undergoing prosthetic rehabilitation. These data are supported by the high frequency of clinical use of ambulatory PerBOMs reported by participants. The TUGT is overall the most reportedly used PerBOM by HCPs, and is used clinically by the majority of participants. Furthermore, most participants who did not use this PerBOM clinically were aware of it, suggesting it is a recommended PerBOM in clinical practice.
The ambulatory PerBOM most frequently used by participants, rated by the largest number of participants (n=72) and with the highest score of usefulness, is the TUGT. This score may to be the most reliable score of usefulness of the PerBOM ratings due to the largest number of participants rating it. Additionally, the 2MWT (n=57) had a similar median usefulness score, therefore demonstrating that both PerBOMs are useful for HCPs. The 6MWT (n=48) also had a high usefulness score, but the BBS provided more mixed results, indicating that HCPs in prosthetic rehabilitation centres use the available PerBOMs regularly and find them clinically relevant for patients who have the goal of ambulation or are currently ambulating. Overall, more participants provided a rehabilitation intervention to ambulatory patients who had an amputation than to non-ambulatory patients. In the early stages after amputation, wheelchair rehabilitation is the most common rehabilitation intervention provided to the non-ambulatory patient. Moreover, the data suggest that there are limited rehabilitation services for non-ambulatory patients. Future research may focus on exploring new rehabilitation interventions or services for this under-served population of patients.
Strengths and limitations
This is the first anonymous scoping survey study to explore the current use of PerBOMS by HCPs working with patients who have undergone an amputation due to vascular disease. This study builds on previous research, which has identified all PerBOMs for patients who have undergone an amputation due to vascular disease. Additional strengths include using conditional questioning, which has enabled individuals who were most appropriate to be directed to the correct questions in the survey. This is likely to have improved the completion rate and ensured that the survey length was as short as possible for participants.
The limitations of this study include the small study cohort, with 125 responses despite 860 initial views from the first page. Furthermore, this is a voluntary research study using convenience sampling methodology and therefore, due to sampling methodology, there is a self-selection bias towards research-interested HCPs and a bias towards physiotherapy HCPs in this study. However, despite the broad distribution of this survey to different groups of HCPs and 860 views on the survey’s first page, the small numbers limit the generalisability of this study. These small numbers of participants also reduce the reliability of the results from the subgroup analysis. It could be that, although physiotherapists were the largest professional group within this study, it may be a reflection of the specialist expertise of HCPs who work with this patient cohort and use outcome measures within their clinical practice.
Conclusion
Ambulatory PerBOMs including the TUGT and 2MWT are commonly used in clinical practice and are found to be useful by HCPs. Non-ambulatory PerBOMs including the TFP are less used in clinical practice. Future research may focus on exploring the reasons for the underuse of current PerBOMs with the non-ambulatory patient population. Pending further research and evidence, there may be a clinical need for the development of a meaningful PerBOM for vascular amputees that can be used throughout the patient journey.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(4):199-207
Publication date:
August 18, 2025
Author Affiliations:
1. Department of Cardiovascular Sciences, College of Life Sciences, University of Leicester, Glenfield Hospital, Leicester, UK
2. Leicester Vascular Institute, University Hospitals of Leicester NHS Trust, Glenfield Hospital, Leicester, UK
3. National Institute for Health Research Leicester Biomedical Research Centre, The Glenfield Hospital, Leicester, UK
4. Centre of Exercise and Rehabilitation Sciences, Leicester NIHR Biomedical Research Centre-Respiratory, University Hospitals of Leicester NHS Trust, Leicester, UK
5. Department of Respiratory Sciences, University of Leicester, Leicester, UK
6. Department of Population Health Sciences, College of Life Sciences, University of Leicester, Leicester, UK
Corresponding author:
Amirah Essop-Adam
Department of Cardiovascular Sciences, College of Life Sciences, University of Leicester, Glenfield Hospital, Groby Road, Leicester, LE3 9QP, UK
Email: [email protected]











