WINNING ESSAYS
Rouleaux Club Winning Essay 2024
The Rouleaux Club run an annual essay competition to help promote interest in vascular surgery. Entrants are asked to write 1,500 words on one of three topics selected by the RC Executive. The essays are marked by the committee and the prizes are awarded to the best essay at the annual Vascular Society meeting. There are two prize categories, one for medical students and another for junior doctors. Following the Vascular Societies GB&I Annual Scientific Meeting, the winning essays will be published in the journal.
DOCTOR CATEGORY
Will there ever be a place for robotic vascular surgery in the United Kingdom?
Alex Leslie Starkey, North West (Lancashire)
Introduction
Robotic surgery is now widespread among urological, general surgical and gynaecological centres, but remains poorly-established in UK vascular surgery.1,2 Despite the recognized benefits of enhanced operative precision and growing evidence of favourable outcomes in robotic-assisted abdominal procedures, open or endovascular techniques remain the standard in the UK.3,4 An increasingly old and comorbid UK population means that the need for precise, safe and uncomplicated vascular surgery has never been greater, with robotic surgery offering demonstrable promise in at least some of these domains.5 However, technical limitations, National Health Service (NHS) sustainability targets, funding crises, and historically-high waiting lists for treatment all create potential barriers to the adoption of this still relatively novel technology among UK vascular centres. This review explores why robotic surgery is likely to continue struggling to gain a foothold in UK vascular care, despite potential benefits.
Minimally invasive techniques and vascular surgery
Compared with the PUMA machine, which performed the first robotic neurosurgical biopsies in 1985, modern-day surgical robots are incredibly sophisticated and versatile.6,7 Between 2016 and 2019, 86.2% of radical prostatectomies were performed robotically, and integration of robotic surgical techniques has also continued to progress in other surgical disciplines.2,8,9 The Royal College of Surgeons now publishes specific guidance on the adoption of robotic surgery, regarding the document as a ‘pathway to the future’.10 Despite this, competency in robotic surgery has yet to become a standardised part of surgical training, and opportunities are not equitable across different hospitals and deaneries.11
Robotics are not the only surgical innovation that vascular surgeons have been slow to adopt: the specialty continues to lag behind others in its use of laparoscopy, which is utilised for only a small proportion of cases in selected centres.1 To this end, most evidence for laparoscopic efficacy in vascular surgery comes in the form of case series, and randomised-control trials are lacking.12 Robotic-assisted vascular surgery unfortunately looks set to follow a similar pattern, with most published case series originating from a small number of vascular centres with a particular interest in robotics, most notably the department of Štádler et al. in Prague.1,13–15
The lack of significant progress in robotic vascular surgery in the UK may be surprising to some, given how quickly endovascular techniques were adopted as standard practice. In the year to date, 62% of UK abdominal aortic anneursym (AAA) repairs were performed endovascularly.4 Why, then, has robotic vascular surgery failed to fully establish itself? The incorporation of endovascular technology into everyday practice disproves any notion that vascular surgeons are Luddites, and hence other factors must be at play.
Technical considerations
From a technical standpoint, the ability to sense pressure on delicate and easily-friable tissues is a key aspect of performing safe vascular procedures. While open and laparoscopic surgeries allow surgeons to sense tissue pressure directly or indirectly, this capability is not yet available in current robotic systems.16 Tissue handling errors account for a large proportion of mistakes made by surgical trainees and can lead to significant tissue damage.17,18 Fortunately, this important limitation may soon be overcome, with the upcoming Da Vinci 5 robot promising to deliver the first ever haptic feedback system in a surgical robot.7
Patient factors may also influence the suitability of robotics for performing vascular procedures. Robotic abdominal surgery requires the creation of pneumoperitoneum, which is potentially dangerous for the sizeable number of vascular patients suffering from obstructive lung disease.19 For patients who have undergone multiple previous procedures, intraabdominal adhesions may also lead to operative difficulties.1 Endovascular or open surgery may therefore remain a more suitable choice for these patients, even if robotic technology continues to advance.
Conversely though, some patients potentially stand to gain significantly from robotic surgery. Younger patients keen to avoid a laparotomy scar – but also at risk from repeated irradiation during typical endovascular aneurysm repair (EVAR) follow-up scans – could benefit from similar outcomes to open surgery without the usual cosmetic implications.1,16 Minimally invasive surgery also carries a lower risk of incisional hernia, may reduce the need for in-hospital analgesia, and often allows for earlier discharge.20-22
Surgeons themselves also have the opportunity to benefit from wider use of robotic systems. Reduced postural demand when operating from a robotic console could lower the risk of developing occupation-related musculoskeletal conditions, and the ability to perform surgery remotely could pave the way for more flexible working arrangements across multiple sites.1,23 Tremor-reduction systems present in many modern surgical robots can lower the risk of handling errors, and novel blood vessel detection systems may help to prevent iatrogenic injury.5 Additionally, while 3D laparoscopy cameras do exist, they are yet to fully replace their 2D counterparts – despite the European Association for Endoscopic Surgery recommending their use.24 Modern surgical robots feature 3D viewing as standard.1 Owing to these benefits, robotic vascular surgery may succeed in cases where endovascular procedures have repeatedly failed.25
Specific vascular procedures may be more amenable to robotics than others, and to this end the adoption of robotic technology in the UK may also depend on the type of work undertaken by specific regional departments. Multiple studies have shown promise in treating median arcuate ligament syndrome (MALS) robotically, whereas robotic iliac aneurysm repairs – although demonstrably possible – have entailed significant operative and vessel-clamping times.26-28 For smaller departments that see conditions like MALS less frequently, robotic technology may be of lesser benefit.
Political and environmental considerations
Whilst the UK NHS has a proud history of innovation, it and a large proportion of the population it serves remains in financial difficulty; which can make the acquisition and use of expensive new technologies politically contentious.29 The ROLARR randomised control trial (RCT) found no significant benefits to robotic treatment of rectal cancer versus laparoscopic surgery, despite costing an average of £980 more per patient.30 Moreover, this figure did not even include the costs of acquiring and maintaining the robots, which can be substantial.1 The findings highlight the need for new good-quality research to assess the efficacy of robotic vascular surgery, before any action to promote it’s wider use in the UK.
According to the most recent figures, only 31.6% of surgeries performed following AAA screening were completed within the UK government’s target of 8 weeks, and waiting lists remain a significant problem for the NHS.31 In addition to being generally more expensive, robotic surgeries tend to take longer than their open or laparoscopic alternatives.1,30 In this political setting, proposing the use of a slower operative technique that could result in fewer per-day procedures would likely attract controversy.
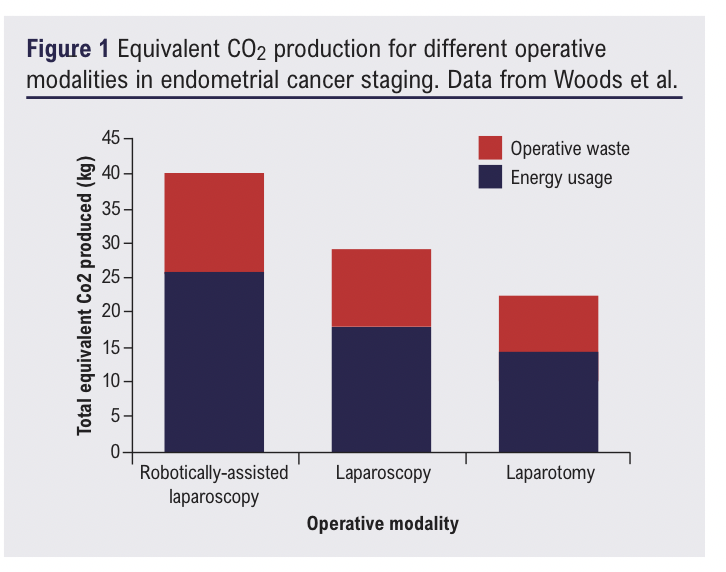
The NHS also has a clear vision regarding its environmental future, aiming to be ‘carbon neutral’ by 2040.32 This presents a considerable problem for those advocating for the expansion of robotic surgery; which has been shown to generate significantly more carbon dioxide (CO2) equivalent than both laparoscopy and laparotomy.33-35 To align with long-term sustainability goals, robotic surgery would need to become significantly more efficient both in terms of operative waste and energy consumption. These key constituents of total CO2 contributions are shown in Figure 1.
Conclusions
Despite the significant role that robotic surgery plays in other disciplines, there remains insufficient evidence to suggest that it will make an impactful contribution to the future of UK vascular surgery. The widespread adoption of EVAR shows that UK vascular surgeons are adaptive to change and welcoming of new technology if there is robust evidence for patient or system benefit, but this remains largely absent for robotic vascular surgery. Whilst it is conceivable that an improved evidence base could encourage UK vascular surgeons to utilise robotics to a greater degree, figuratively and literally buying-in to a costly, less-sustainable and resource-demanding technology would almost certainly not be without controversy. For certain niche procedures, robotic vascular surgery may be the treatment of choice in larger centres with existing access to surgical robots. On a broader scale, however, UK vascular surgery is unlikely to undergo any meaningful robotic revolution.
References
1. Štádler P, Dorosh J, Dvořáček L, Vitásek P, Matouš P, Lin JC. Review and current update of robotic-assisted laparoscopic vascular surgery. Semin Vasc Surg 2021;34(4):225–32. https://doi.org/10.1053/j.semvascsurg.2021.10.007
2. Lam K, Clarke J, Purkayastha S, Kinross JM. Uptake and accessibility of surgical robotics in England. International Journal of Medical Robotics and Computer Assisted Surgery 2021;17(1):1–7. https://doi.org/10.1002/rcs.2174
3. Kawka M, Fong Y, Gall TMH. Laparoscopic versus robotic abdominal and pelvic surgery: a systematic review of randomised controlled trials. Springer. Surgical Endoscopy 2023;37:6672–81. https://doi.org/10.1007/s00464-023-10275-8
4. Vascular Services Quality Improvement Program. National Vascular Registry Dashboard [Internet]. 2024 [cited 2024 Sep 27].
Available from: https://rcs-ceu.shinyapps.io/NVR_dashboard/
5. Lengyel BC, Chinnadurai P, Corr SJ, Lumsden AB, Bavare CS. Robot-assisted vascular surgery: literature review, clinical applications, and future perspectives. Springer Nature. J Robotic Surg 2024;18:328. https://doi.org/10.1007/s11701-024-02087-2
6.Kwoh YS, Hou J, Jonckheere EA, Hayati S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng 1988;35(2):153–60. https://doi.org/10.1109/10.1354. Available from: https://pubmed.ncbi.nlm.nih.gov/3280462/
7. Intuitive. Haptic feedback in Intuitive’s da Vinci 5 [Internet]. [cited 2024 Sep 27]. Available from: https://www.intuitive.com/en-us/about-us/newsroom/Force%20Feedback
8. British Association of Urological Surgeons. Radical Prostatectomy Registry 2016-2019 National Summary Results. 2019.
9. Morton AJ, Simpson A, Humes DJ. Regional variations and deprivation are linked to poorer access to laparoscopic and robotic colorectal surgery: a national study in England. Tech Coloproctol 2024;28(1). https://doi.org/10.1007/s10151-023-02874-3. Available from: /pmc/articles/PMC10713759/
10. Royal College of Surgeons England. Robotic-Assisted Surgery: A Pathway to the Future – A Guide to Good Practice [Internet]. 2023. Available from: www.rcseng.ac.uk/standardsandguidance
11. Boal MWE, Afzal A, Gorard J, Shah A, Tesfai F, Ghamrawi W, et al. Development and evaluation of a societal core robotic surgery accreditation curriculum for the UK. J Robot Surg 2024;18(1). https://doi.org/10.1007/s11701-024-02062-x
12. Howard AQ, Bennett PC, Ahmad I, Choksy SA, Mackenzie SIP, Backhouse CM. Introduction of laparoscopic abdominal aortic aneurysm repair. John Wiley and Sons Ltd. British Journal of Surgery 2015;102(4):368-74.
13. Khajuria A. Robotics and surgery: A sustainable relationship? World J Clin Cases 2015;3(3):265.
14. Štádler P, Dvořáček L, Vitásek P, Matouš P. Robot assisted Aortic and Non-aortic Vascular Operations. European Journal of Vascular and Endovascular Surgery 2016;52(1):22–8. https://doi.org/10.1016/j.ejvs.2016.02.016
15. Coggia M, Di Centa I, Javerliat I, Alfonsi P, Kitzis M, Goëau-Brissonnière OA. Total laparoscopic abdominal aortic aneurysms repair. Journal of Vascular Surgery 2005;42(5):906–10. https://doi.org/10.1016/j.jvs.2005.06.035
16. Rusch R, Hoffmann G, Rusch M, Cremer J, Berndt R. Robotic-assisted abdominal aortic surgery: evidence and techniques. Springer Nature. Journal of Robotic Surgery 2022;16:1265–71. https://doi.org/10.1007/s11701-022-01390-0
17. Tang B, Hanna GB, Cuschieri A. Analysis of errors enacted by surgical trainees during skills training courses. Surgery 2005;138(1):14–20.
https://doi.org/10.1016/j.surg.2005.02.014. Available from: https://pubmed.ncbi.nlm.nih.gov/16003310/
18. Khan AF, Macdonald MK, Streutker C, Rowsell C, Drake J, Grantcharov T. Tissue stress from laparoscopic grasper use and bowel injury in humans: establishing intraoperative force boundaries. BMJ Surg Interv Health Technol 2021;3(1). https://doi.org/10.1101/2021.02.19.21252109
Available from: https://pubmed.ncbi.nlm.nih.gov/35047803/
19. Qureshi MA, Greenberg RK, Mastracci TM, Eagleton MJ, Hernandez A V. Patients with chronic obstructive pulmonary disease have shorter survival but superior endovascular outcomes after endovascular aneurysm repair. J Vasc Surg 2012;56(4):911-19.e2. https://doi.org/10.1016/j.jvs.2012.02.055
20. Cochennec F, Javerliat I, Di Centa I, Goëau-Brissonnière O, Coggia M. A comparison of total laparoscopic and open repair of abdominal aortic aneurysms. J Vasc Surg 2012;55(6):1549–53. https://doi.org/10.1016/j.jvs.2011.11.131
21. Sheng S, Zhao T, Wang X. Comparison of robot-assisted surgery, laparoscopic-assisted surgery, and open surgery for the treatment of colorectal cancer A network meta-analysis. Lippincott Williams and Wilkins. Medicine 2018;97(34):e11817. https://doi.org/10.1097/md.0000000000011817
22. Coggia M, Javerliat I, Di Centa I, Alfonsi P, Colacchio G, Kitzis M, et al. Total laparoscopic versus conventional abdominal aortic aneurysm repair: A case-control study. J Vasc Surg 2005;42(5):906–10. https://doi.org/10.1016/j.jvs.2005.06.035
23. Sherif YA, Adam MA, Imana A, Erdene S, Davis RW. New and updated applications for robotic surgery in plastic surgery: Remote Robotic Surgery and Virtual Education Platforms: How Advanced Surgical Technologies Can Increase Access to Surgical Care in Resource-Limited Settings. Semin Plast Surg 2023;37(3):217. https://doi.org/10.1055/s-0043-1771301. Available from: /pmc/articles/PMC10569862/
24. Arezzo A, Vettoretto N, Francis NK, Bonino MA, Curtis NJ, Amparore D, et al. The use of 3D laparoscopic imaging systems in surgery: EAES consensus development conference 2018. Surg Endosc 2019;33(10):3251–74. https://doi.org/10.1007/s00464-018-06612-x
25. Davila VJ, Velazco CS, Stone WM, Fowl RJ, Abdul-Muhsin HM, Castle EP, et al. Robotic inferior vena cava surgery. J Vasc Surg Venous Lymphat Disord 2017;5(2):194–9. https://doi.org/10.1016/j.jvsv.2016.08.003. Available from: https://pubmed.ncbi.nlm.nih.gov/28214486/
26. Gerull WD, Sherrill W, Awad MM. Robotic median arcuate ligament release: management algorithm and clinical outcomes from a large minimally invasive series. Surg Endosc 2023;37(5):3956–62. https://doi.org/10.1007/s00464-022-09545-8
27. Simioni A, Yi J, Wohlauer M V., Malgor RD, Jacobs DL, Pratap A. Robotic-assisted Median Arcuate Ligament Release: Phrenoesophageal Membrane Preserving Step-by-Step Technique and Early Outcomes. J Vasc Surg 2023; 77(6):e162–3. https://doi.org/10.1016/j.jvs.2023.03.224
28. Colvard B, Georg Y, Lejay A, Ricco JB, Swanstrom L, Lee J, et al. Total robotic iliac aneurysm repair with preservation of the internal iliac artery using sutureless vascular anastomosis. J Vasc Surg Cases Innov Tech 2019; 5(3):218–24. https://doi.org/10.1016/j.jvscit.2019.01.001
29. Meadows J, Montano M, Alfar AJK, Başkan ÖY, De Brún C, Hill J, et al. The impact of the cost-of-living crisis on population health in the UK: rapid evidence review. BMC Public Health 2024;24(1). https://doi.org/10.1186/s12889-024-17940-0. Available from: https://pubmed.ncbi.nlm.nih.gov/38388342/
30. Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Robotic-assisted surgery compared with laparoscopic resection surgery for rectal cancer: the ROLARR RCT. Efficacy and Mechanism Evaluation 2019;6(10):1–140. https://doi.org/10.3310/eme06100
Available from: https://pubmed.ncbi.nlm.nih.gov/31556981/
31. NHS England. AAA standards report 2023 to 2024 – GOV.UK [Internet]. 2024 [cited 2024 Sep 27]. Available from: https://www.gov.uk/government/statistics/ abdominal-aortic-aneurysm-screening-standards-report-2023-to-2024/aaa-standards-report-2023-to-2024–2#aaa-standards
32. NHS England. Delivering a “Net Zero” National Health Service. 2022 Jul.
33. Papadopoulou A, Kumar NS, Vanhoestenberghe A, Francis NK. Environmental sustainability in robotic and laparoscopic surgery: Systematic review. Oxford University Press. British Journal of Surgery 2022;109:921–32. https://doi.org/10.1093/bjs/znac191
34. Chan KS, Lo HY, Shelat VG. Carbon footprints in minimally invasive surgery: Good patient outcomes, but costly for the environment. World J Gastrointest Surg 2023;15(7):1277–85. https://doi.org/10.4240/wjgs.v15.i7.1277
35. Woods DL, Mcandrew T, Nevadunsky N, Hou JY, Goldberg G, Yi-Shin Kuo D, et al. Carbon footprint of robotically-assisted laparoscopy, laparoscopy and laparotomy: A comparison. International Journal of Medical Robotics and Computer Assisted Surgery 2015;11(4):406–12. https://doi.org/10.1002/rcs.1640
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(3):160-162
Publication date:
May 29, 2025











