PROTOCOL
The use of non-steroidal anti-inflammatory drugs for the prevention and reduction of pain following superficial venous incompetence treatment: a systematic review protocol
Vedanayagam B,1 Mohamed AH,1,2 Chua W,1 Stalinland T,2 Curtis D,3 Chetter I1,2
Plain English Summary
Why we are undertaking this research: Enlarged and twisted veins just under the skin in the legs (varicose veins) are common and often cause problems such as pain, swelling, itching and wounds that are hard to heal (ulcers). The most common treatment for varicose veins is to use heat or chemicals to seal the veins shut. Approximately 30% of patients report prolonged pain after such treatments. Reducing this pain would improve patients’ quality of life and reduce associated healthcare costs. A short course of painkillers following treatment may minimise the pain, but this is not currently routine. Non-steroidal anti-inflammatory drugs (NSAIDs) are a group of painkillers which can be bought commonly over-the-counter and include ibuprofen and aspirin. We want to know if a routine short course of NSAIDS reduces the pain patients experience after treatment for varicose veins.
What we aim to do: To investigate the effect of NSAIDs on pain following treatment for varicose veins, we are going to do a systematic review. A systematic review is a way of bringing together the results from existing studies to decide if a treatment is effective or not. This paper describes how we will bring together all existing studies on painkillers after varicose vein treatments to determine whether they should be used in routine practice.
What this means: The results from this review will tell us if NSAIDs should be used in routine practice to reduce or prevent pain after varicose vein treatment, or if more research is needed. It will also allow other researchers to repeat the systematic review if they wish.
Abstract
Introduction: Post-procedural pain is a common complication following interventional treatments for patients with superficial venous incompetence (SVI). Currently, analgesia is not routinely prescribed following treatment. Simple analgesia in the form of non-steroidal anti-inflammatory drugs (NSAIDs) can be administered. This is a protocol for a systematic review of the studies on the use of NSAIDs following SVI treatment for post-procedural pain.
Methods: A systematic review will be conducted on the use of NSAIDs for post-procedural pain following SVI treatment in accordance with PRISMA guidelines. A search of Ovid MEDLINE, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) databases will be carried out to search for terms including ‘varicose veins’, ‘non-steroidal anti-inflammatory’, ‘ibuprofen’ and ‘post-procedural pain’. The primary outcome of the review will be post-procedural pain, defined as pain occurring within the first six weeks following SVI treatment. The secondary outcomes will be patient adherence to NSAID treatment, reported complications from NSAID treatment and mean time to return to normal daily activities/work. All prospective and retrospective studies considering the use of NSAIDs to reduce and prevent pain following SVI treatments will be included. The Covidence systematic review software will be used for the screening and selection of studies. Data extraction will be performed using a dedicated Excel spreadsheet. The risk of bias of included studies will be assessed using tools recommended by Cochrane for both randomised and non-randomised studies. The GRADE tool will be used to assess the quality of the evidence.
Conclusion: This systematic review aims to assess and summarise the evidence for the use of NSAIDs for pain following SVI treatment. The findings will inform us whether NSAIDs should be used routinely or whether further research is needed.
Introduction
Superficial venous incompetence (SVI) is among the most common chronic diseases in adults. Approximately one-third of the general population is affected, with the main risk factors being older age, parity, obesity and family history.1–3 The disease commonly manifests as varicose veins, which are tortuous and dilated superficial veins in the lower extremities. It also leads to symptoms in the lower limbs such as pain, itching, swelling and heaviness.4,5 Clinical assessment is performed using the Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification, with varicose veins being at the C2 Clinical stage and active venous ulceration being the highest Clinical class (C6).6 Other serious complications include bleeding, eczema, phlebitis and venous thromboembolism.7-9 SVI symptoms negatively impact the physical, social and psychological aspects of a patient’s quality of life (QoL), and international guidelines recommend treating all patients with symptomatic SVI.10
Interventional treatments of SVI include thermal and non-thermal minimally invasive approaches as well as open surgery. These procedures are effective at relieving symptoms, improving QoL and reducing disease complications.11,12 However, they are associated with recognised post-procedural complications. Major but rare complications include deep vein thrombosis and pulmonary embolism.13,14 Nearly all patients experience early post-procedural pain and discomfort, which resolves within 1–2 weeks.15,16 However, persistent post-procedural pain is experienced by up to 30% of patients following SVI treatment, and this can last up to 6 weeks and is likely associated with inflammation of residual thrombosed varicose tributaries.17 Early post-procedural pain is an appropriate response to the procedural insult; however, prolonged post-procedural pain and tenderness are pathological, and attempts should be made to minimise this phenomenon.
Most patients undergoing SVI treatment are working adults who are otherwise fit, and, therefore, a delay in post-procedural recovery of 6 weeks represents a significant illness.18 Moreover, prolonged pain can result in a significant socioeconomic impact as it prevents the return to normal daily activities such as exercise or work. This, in turn, causes distress and leads to unplanned visits to health professionals and additional strain on stretched healthcare services. The reported frequency of this phenomenon and its impact on patients warrant an assessment of the literature to find strategies to address it.
Administration of non-steroidal anti-inflammatory drugs (NSAIDs) is therefore a potential solution to this persistent pain. NSAIDs have dual activity, providing analgesia as well as reducing the body’s inflammatory response. This may reduce the severity of symptoms, allowing patients to return to normal daily activities. Additionally, early administration may also prevent the activation of this persistent pain cascade by reducing inflammation. There is evidence for the use of NSAIDs to treat similar short/medium-term inflammatory processes such as musculoskeletal pain and in other surgical and non-surgical settings.19-21 Therefore, a systematic review of the literature to ascertain the effect of NSAID use on post-procedural pain and patient recovery following SVI treatment is warranted.
Methods
This systematic review protocol is written in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines and is registered with the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42024598078).22 A systematic review of the literature will be conducted in line with Cochrane’s recommendations for performing systematic reviews of interventions.23 The objective of the systematic review is to identify and synthesise the literature on whether NSAIDs reduce pain following SVI treatment.
Study eligibility criteria
All randomised controlled trials (RCTs), prospective and retrospective studies evaluating the use of NSAIDs in reducing post-procedural pain in patients with SVI of either sex following interventional treatment are eligible for inclusion. The study population are symptomatic patients undergoing interventional treatment for SVI. Only invasive interventional treatments recommended by international bodies such as the European Society for Vascular Surgery (ESVS) for SVI will be eligible for inclusion, such as endovenous laser and radiofrequency ablation, foam sclerotherapy, cyanoacrylate adhesive ablation, mechanochemical ablation and varicose vein surgical stripping.10 Compression therapy and lifestyle advice will not be included as they are considered non-invasive.
The study intervention will consist of the administration of NSAID medication shortly after SVI treatment. All NSAID types and formulations are acceptable interventions. NSAIDs given before SVI treatment will not be eligible for inclusion. The duration of the course of NSAID treatment will be no less than 1 week and not longer than 8 weeks. Acceptable comparators include the use of analgesia other than NSAIDs or not offering any systemic analgesic medication. Comparison of types of NSAIDs is also acceptable.
Studies to be included must be peer-reviewed English language studies. The language restriction is because we do not have the resources to translate manuscripts. Book chapters and conference abstracts will be excluded. No date restrictions will be applied. Unpublished data that meet the inclusion criteria are acceptable to be included. Studies assessing pain before and after SVI treatment for the aim of assessing symptom resolution are not eligible for inclusion.
Outcomes
Post-procedural pain, specifically in the first 6 weeks following SVI treatment, will be the primary outcome. There is no consensus on the duration of post-procedural pain; thus, a window of 6 weeks was chosen pragmatically in order to maximise eligible data but not capture pain that may be deemed as chronic. Pain must be measured using validated patient subjective pain scores such as the 100 mm Visual Analogue Scale (VAS), Numerical Rating Scale (NRS), Verbal Rating Scale (VRS), FACES Pain Rating Scale or other conventional and accepted pain measurement tools.24-27 Studies that report post-procedural pain >6 weeks following varicose veins treatment will be excluded unless they also report pain in the first 6 weeks.
The secondary outcomes will be patient adherence to NSAID treatment, reported complications from NSAID treatment (including but not limited to abdominal pain, indigestion, cough, nausea, shortness of breath and headache), and mean time to return to normal daily activities/work.
Search strategy
Searches will be conducted on Ovid MEDLINE, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) electronic databases from inception to December 2024. Literature searches will be performed under the supervision of qualified medical librarians (DC, TS). References of studies included in the review will be examined for additional eligible studies that may have been missed from the literature searches.
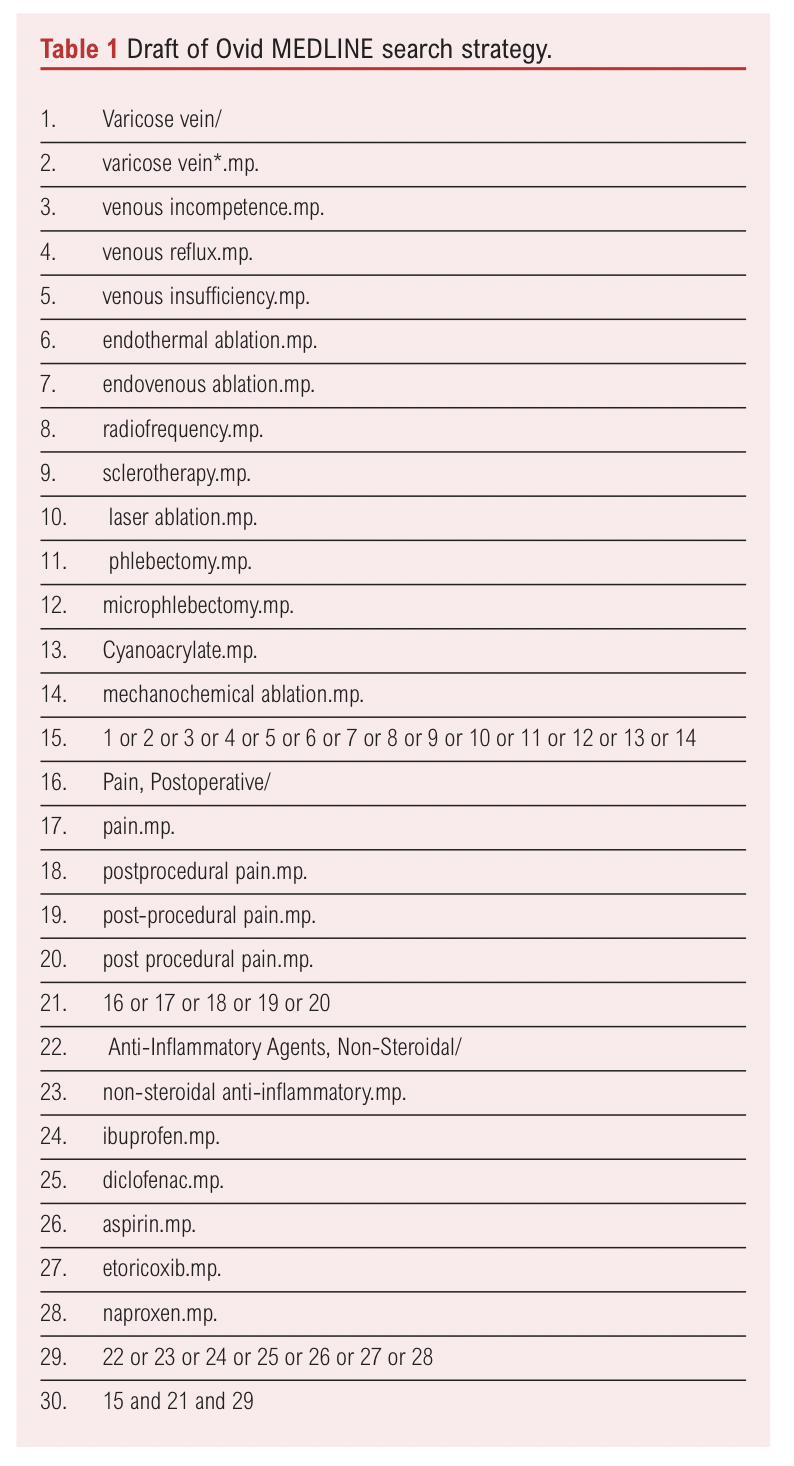
The databases will be searched for studies reporting the use of NSAIDs following SVI interventional treatment using keywords, equivalent words and Medical Subject Headings (MeSH) terms to maximise search sensitivity. Search terms will include but are not limited to ‘non-steroidal anti-inflammatory’, ‘ibuprofen’, ‘varicose veins’ and ‘postprocedural pain’.
An example search strategy for the search on Ovid MEDLINE is outlined in Table 1. A similar approach will be employed for other databases, taking into account variations in acceptable search terms between databases.
In addition to the databases, clinical trial registers such as clinicaltrials.gov will be searched for ongoing studies. If any abstracts of ongoing clinical trials or unpublished data meet the inclusion criteria, then the authors will be contacted for results, if available. Grey literature will not be searched in this review.
Study selection
The Covidence systematic review software (2024, Veritas Health Innovation, www.covidence.org) will be used for study screening and selection. The search results will be uploaded to Covidence, followed by automatic duplicate identification and removal. Two assessors will independently review the literature search results and screen studies that meet the inclusion criteria based on the title and abstract. If studies are deemed eligible, they will be screened further using a full-text review by the same two independent reviewers. The reviewers will be blinded to each other’s decisions. Any discrepancies will be resolved by consensus between the two reviewers or arbitration of a third reviewer.
A PRISMA flow diagram will be produced to convey information such as the number of search hits, the number of duplicates automatically removed, the number of titles, abstracts and full texts reviewed, the number of studies excluded following full-text review with the reasons for exclusion displayed and ultimately the number of studies included in the systematic review.
Data collection and synthesis
Two reviewers will independently extract data from the studies identified onto two separate Microsoft Excel spreadsheets (Microsoft® Corporation, 2024) using specifically designed data extraction forms. Once the extraction has been completed, the reviewers will compare the results. If there are any discrepancies, these will be resolved again through consensus. If any clarification is needed, it will be resolved by obtaining and confirming data from investigators and inputting it into the final form.
Data will be collected on study characteristics including study design and sample size, participant demographics including age, sex and comorbidities, a description of the intervention(s) and comparators, if any, adverse events, length of follow-up and findings related to primary and secondary outcome data. Data on study characteristics will include information to make a judgement on the quality of the study. If available, conflicts of interest, funding for the study and other potential sources of bias will be reported. RCTs and non-randomised studies will be reported separately. For each study included, a table will be provided outlining the key characteristics and findings.
Quantitative outcome data analysis will be conducted using Cochrane’s RevMan software program.28 First, the clinical heterogeneity will be reviewed, specifically the patient demographics, comorbidities, types of interventions, follow-up duration and outcomes. If the criteria for clinical homogeneity are satisfied, then statistical heterogeneity will be assessed using χ2 and I2 tests and associated p values. χ2 represents the estimate of the variance of true treatment effects between the trials. I2 is an estimate of the proportion of variability that is due to trial heterogeneity. Data from different interventional treatments of SVI will be analysed separately. Meta-analyses will be performed for studies that are deemed clinically homogenous. Dichotomous outcomes will be presented in a forest plot with risk ratios and 95% CI, whereas continuous outcomes will be presented as mean difference (MD) or standardised mean difference (SMD) with 95% CI. Data from homogeneous single-arm cohort studies will be combined and presented as a mean with a 95% CI for continuous outcomes or proportion with a 95% CI for categorical outcomes, or a hazard ratio with a 95% CI for time-to-event data. Data from RCTs will be presented separately from observational studies. A narrative synthesis will be provided for any included studies that cannot be included in quantitative data analysis.
Bias risk assessment
For RCTs, two independent reviewers will assess the risk of bias using Cochrane’s risk-of-bias tool for randomised trials (RoB-2).29 It assesses the risk of bias across five domains, including bias arising from the randomisation process, bias due to deviations from the intended interventions, bias due to missing outcome data, bias in the measurement of outcome and bias in the selection of the reported result. Within each domain there is a series of signalling questions, and the responses are combined to make a final judgement about the risk of bias for each domain. If there are any discrepancies between the two reviewers, this will be resolved by a consensus or arbitration with a third reviewer. A Microsoft Excel table will be used to implement the RoB-2. Any studies with an outcome of high risk of bias will be excluded from quantitative data analysis and synthesis.
The risk of bias in non-randomised studies will be assessed using the modified Downs and Black checklist, which assesses different components of the methodology.30 It comprises 27 questions which can be answered using a ‘yes’, which equates to 1 point, ‘no’ or ‘unable to determine’, each of which is 0 points. The maximum score is 28 points, with a higher score indicating better quality.
The presence of publication bias and selective outcome reporting will be explored further using funnel plots.
The overall quality of the evidence will be assessed by using the Grading of Recommendations, Assessments, Development and Evaluations (GRADE) tool.31 First, the study design will be considered. Then the evidence will be downgraded or upgraded based on five categories: the risk of bias, inconsistency, indirectness, imprecision and publication bias. The evidence can be rated ‘high’, ‘moderate’, ‘low’ or ‘very low’.
Discussion
This protocol outlines a systematic review that aims to identify and summarise the evidence base for and safety of NSAIDs in relieving pain following SVI treatment. The findings will be used to inform current practice or the design of future studies to investigate how NSAIDs can be best utilised to optimise patient recovery following SVI treatment. The NHS in England performs approximately 35,000 procedures to treat SVI each year.18 Most of these patients are working-age adults for whom delays in recovery impact employment and care duties. Currently, post-procedural care and pharmacotherapy are guided by clinician preferences, and potentially a third of patients are negatively impacted by this practice.17 Data from this review and subsequent studies will provide evidence to support a standardised care package to optimise recovery post-SVI treatment.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;5(1):23-27
Publication date:
November 17, 2025
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
2. Hull University Teaching Hospitals, Hull, UK
3. Hull York Medical School, York, UK
Corresponding author:
Benita Vedanayagam
Academic Vascular Surgical Unit, Tower Block, Hull Royal
Infirmary, Hull HU3 2JZ, UK
Email: benita.vedanayagam@ nhs.net











