ABSTRACTS
VASGBI Annual Scientific Meeting 2025, London, 15-16th September, oral presentation top abstracts
Authors of the top scoring abstracts submitted were given the opportunity to give an oral presentation of their work during our free paper session. The papers by Dr Ian Young and Dr Michael Nesbitt were joint first prize winners.
An audit of the impact of a joint surgical and anaesthetic pre-op assessment clinic for abdominal aortic aneurysms
Dr Michael Nesbitt, Dr Sneha Betkekar, Mr Andrew Batchelder, Dr Rishie Sinha, Dr David Evans, Dr Delme Luff, Dr Oliver Morgan
Nottingham University Hospitals NHS Trust – Queens Medical Centre
Introduction
Following recommendations made by the national abdominal aortic aneurysm quality improvement programme (AAAQIP), that we should adopt a multi-disciplinary approach to pre-op assessment, we introduced a joint surgical and anaesthetic pre-op assessment clinic for abdominal aortic aneurysms (AAA) in March 2024. In the clinic, all patients are reviewed jointly by a consultant vascular surgeon and a consultant vascular anaesthetist. The aims of this are to improve pre-op multi-disciplinary team (MDT) involvement, in keeping with AAAQIP recommendations, and also to improve the efficiency of our AAA pre-op pathway, measured by the time from referral to surgery and the proportion of patients who undergo elective AAA repair within 8 weeks of assessment.
Methods
We conducted a retrospective audit of the following: 1) Time from referral to review by a consultant vascular surgeon. 2) Time from referral to review by a consultant vascular anaesthetist. 3) Time from referral to surgery (open or endovascular AAA repair). We compared patients who were referred for surgery in the 6-month period after the clinic started (March – September 2024), to patients who were referred for surgery during the same 6-month period of the previous year (March – September 2023). We also accessed national vascular registry (NVR) data, to analyse our trusts performance against the 8-week target for time from assessment to surgery.
Results
Before clinic set-up (March – September 2023), 29 patients underwent elective AAA repair. The mean time from referral to review by a consultant vascular surgeon was 29 days, mean time from referral to review by a consultant vascular anaesthetist was 80 days, and the mean time from referral to surgery was 161 days (23 weeks).
In comparison, after clinic set-up (March – September 2024), 16 patients underwent elective AAA repair. There were improvements in all 3 areas, but most significantly in the mean time from referral to review by a consultant vascular anaesthetist (21 days vs. 80 days) and the mean time from referral to surgery (63 days vs. 161 days).
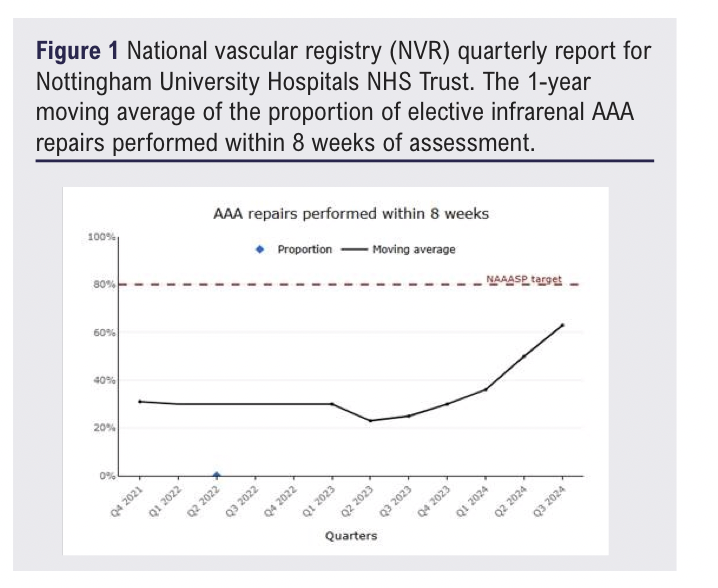
Figure 1 shows the moving average of the proportion of AAA repairs performed within 8 weeks of assessment. It is clear that from the first quarter of 2024 (Q1 2024) onwards, there was a significant improvement in this metric. By the third quarter of 2024 (Q3 2024), over 60% of AAA repairs were performed within 8 weeks, compared to only 34% in Q1 2024. This represents a significant improvement in our performance against the 8-week target.
In comparison, the national (United kingdom) performance against the 8-week target for assessment to treatment remained static during the same period (29% in Q1 2024 vs. 34% in Q3 2024).
Conclusion
We have demonstrated that the implementation of a joint surgical and anaesthetic pre-op assessment clinic for AAA, has resulted in substantial reductions in the time from referral to review by a consultant vascular anaesthetist, and the time from referral to surgery. The improved efficiency of our AAA pre-op pathway is reflected in our NVR data, which demonstrates a dramatic improvement in the proportion of patients who undergo surgery within the target timeframe. Ultimately, this should result in fewer AAA ruptures while patients are waiting for surgery.
From Comorbidity to Mortality: Long-Term Outcomes Following Open Thoracoabdominal Aortic Aneurysm Repair in a National Surgical Cohort
Dr Ian Young,1 Dr Alasdair Ruthven,1 Dr Euan McGregor,1 Mr Aryaan Ashraf,2 Mr Orwa Falah1
1The Royal Infirmary of Edinburgh; 2The University of Edinburgh
Introduction
Patients undergoing open thoracoabdominal aortic aneurysm (TAAA) repair frequently present with significant comorbidity. Pre-operative assessment seeks to identify peri-operative risk and ensure functional fitness for surgery. However, it remains unclear whether flagged comorbidities are predictive of future cause-specific mortality, or simply descriptive features of this ageing surgical population. We aimed to examine the long-term relationship between pre-operative comorbidities and eventual causes of death.
Methods
We reviewed all 424 patients who underwent open TAAA repair at the Royal Infirmary of Edinburgh between 1999 and 2022. Patients completed a standardised pre-operative assessment including cardiopulmonary exercise testing, stress echocardiography, CT coronary angiography, and pulmonary function testing. Mortality data, including primary cause of death, were obtained from the Scottish mortality registry and censored in 2024. We analysed the relationship between specific pre-operative comorbidities (cardiovascular, cerebrovascular, respiratory, and renal) and actual causes of death. These were compared to age-matched mortality rates in the general Scottish population.
Results
By 2024, 168 patients (40%) had died. Among those with pre-operative cardiovascular disease, 33% had died, but only 5.8% died from ischaemic heart disease. Of patients with respiratory comorbidity, 43% had died, but only 7.5% from respiratory causes. For those with cerebrovascular disease, 39% had died, but only 10.7% from stroke-related causes. Of those with chronic kidney disease, 32% had died, but only 2.6% from renal failure. In every comorbidity category, more patients died of a different cause than from their flagged comorbidity.
Discussion
Pre-operative comorbidities were not strongly predictive of cause-specific mortality. Most patients died of causes other than the comorbidity identified prior to surgery. These findings suggest that while pre-assessment effectively selects patients with adequate physiological reserve, comorbidities should be interpreted cautiously in predicting long-term outcomes. For multidisciplinary teams, this distinction is important: comorbidities that do not impair functional capacity should not be over-weighted in estimating long-term prognosis following open TAAA repair.
Opioid Requirements Following Elective Open AAA Repair: The Analgesic Impact of Epidural and Spinal Techniques
Dr Kirsty House,1 Dr Rishabh Sethi,2 Dr Lisa Grimes2
1Luton and Dunstable Hospital, Bedfordshire NHS Foundation Trust; 2Addenbrookes Hospital, Cambridge University Hospitals
Effective perioperative analgesia is essential in elective open abdominal aortic aneurysm (oAAA) repair, a procedure associated with high postoperative pain and morbidity. Thoracic epidural analgesia (TEA) has demonstrated reductions in complications, long-term mortality and hospital stay,1-3 lowering delirium incidence through reduced opioid use.4 It is recommended by ERAS and the Society for Vascular Surgery due to benefits in pulmonary and cardiac outcomes, GI bleeds and ICU stay.5
However, TEA carries risks in vascular patients receiving perioperative anticoagulation. 6,7 With ERAS moving away from TEA in favour of spinal techniques in some abdominal procedures, interest has grown in the use of intrathecal analgesia (ITA) for oAAA surgery. Though less common in this setting, ITA may help reduce systemic opioid use.8 This is increasingly relevant in the context of opioid-related adverse effects and the broader opioid crisis.9
We reviewed our local electronic records to evaluate analgesic strategies and postoperative systemic opioid requirements for elective oAAA cases performed between 2019–2024. Patients were classified into three groups: 1) TEA, 2) ITA, and 3) GA alone. Oral morphine equivalent (OME) doses were calculated over the first 72 postoperative hours.
A total of 199 patients met inclusion criteria. Demographics across groups were comparable. TEA was the most frequently employed technique (n=121), with ITA (n=44) and GA (n=43) used less often. TEA patients had the lowest systemic opioid use: median 5mg OME (0-258mg). Median OME was markedly higher in both ITA (274.5 mg) and GA (283.5 mg) groups (149-589mg, 185-463mg).
TEA was associated with significantly reduced opioid consumption compared to GA (p<0.001) and ITA (p<0.001). No significant difference was observed between ITA and GA (p=0.92). There was no significant difference in length of stay across groups (p=0.79), although itshowed wide variation, likely reflecting surgical complexity and patient comorbidities.
While recent literature suggests spinal anaesthesia may match TEA in early postoperative analgesia,10 our data show TEA remains the preferred technique in elective oAAA repair in our centre. In most ITA cases, the choice was due to contraindications or technical failure of epidural placement.
TEA use correlated with a substantial opioid-sparing effect, reinforcing its value in multimodal analgesia for older, comorbid vascular patients, where minimising opioid exposure is critical.3 Conversely, ITA did not confer a significant opioid reduction vs GA. Prior studies have reported superior early pain control with ITA, even over TEA,10 which prompts interest in combined spinal-epidural (CSE) approaches.
OME was used as a proxy for pain scores. Future research should include patient-reported outcomes, such as pain scores, mobility, opioid side effects, and long-term functional recovery.
D Timbrell1, H Tote2, E Dawrant2, H Latham2, J Gudgeon1
1Frimley Park Hospital, Frimley Health NHS Foundation Trust, Surrey; 2University of Sheffield
NT-pro-BNP (N-terminal pro–B-type natriuretic peptide) is a biomarker that may indicate perioperative risk in high-risk patients undergoing non-cardiac surgery.1,2 We sought to identify whether NT-pro-BNP correlated with CPET variables or Clinical Frailty Score (CFS) in our vascular surgical population being considered for abdominal aortic aneurysm (AAA) surgery.
We analysed data from 126 patients being considered for AAA surgery who underwent CPET at our institution in 2024. Variables including peak oxygen uptake (VO2 peak), anaerobic threshold (AT), ventilatory equivalent for carbon dioxide (VE/VCO2), and CFS were extracted from our CPET database. NT-pro-BNP values were collected from the electronic patient record (Epic). NT-pro-BNP values were included if taken within 6 months of the CPET test and prior to surgery. A Spearman’s rank correlation analysis was performed to identify whether a correlation existed between pre-operative NT-pro-BNP and each variable. Statistical analysis was performed using Microsoft Excel.
A total of 126 patients underwent CPET between 1 January and 31 December 2024. Fifty-two were excluded due to unavailable NT-pro-BNP data. Seventy-four patients were analysed. Demographics: male 63/74 (85.1%), mean age 73.3 years (range 57–89 years). Median NT-pro-BNP was 185ng/L (range 25–36,772 ng/L). Mean VO2 peak was 17.1 mL/kg/min (range 7.9–31.0 mL/kg/min). AT data were available for 68/74 patients, with a mean value of 12.5 mL/kg/min (range 6.9–27.3 mL/kg/min). VE/VCO2 was available for 70/74 patients (mean 33.9, range 23–51). CFS was available for 72/74 patients, median score 3 (range 1–7).
Spearman’s correlation coefficients (r3) were:
NT-pro-BNP vs VO2 peak: –0.38
NT-pro-BNP vs AT: –0.14
NT-pro-BNP vs VE/VCO2: +0.23
NT-pro-BNP vs CFS: +0.31
This exploratory analysis suggests a moderate inverse correlation between NT-pro-BNP and VO2 peak, and weaker associations with AT and VE/VCO2. A modest positive correlation was observed between NT-pro-BNP and CFS. These findings support the hypothesis that NT-pro-BNP may reflect broader physiological reserve beyond cardiac function alone. While limited by small sample size and retrospective design, this study suggests NT-pro-BNP could complement existing measures of cardiopulmonary fitness and frailty in perioperative risk stratification for AAA surgery.3
References
1. Kristensen SD, De Hert S, Bueno H, et al. Eur Heart J 2022;43:3826–924.
2. Schmidt C, et al. BMC Anesthesiol 2024;24:113
3. Partridge JS, Harari D, Dhesi JK. Int J Surg 2015;18:57–63.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;5(1):46-48
Publication date:
November 26, 2025











